Prof. Dr. Pham Manh Hung
Scientific Advisor, An Sinh Hospital, Ho Chi Minh City
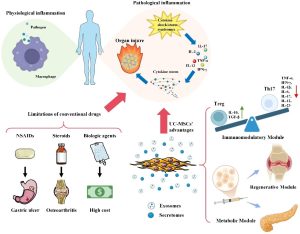
In recent years, mesenchymal stem cells isolated from newborn umbilical cords have been effectively used by many authors to treat chronic inflammatory conditions in several diseases: arthritis, COPD, graft-versus-host disease, chronic hepatitis, etc. (5, 6). Mesenchymal stem cells can be isolated from various tissues in the human body: bone marrow, peripheral blood, adipose tissue, placenta, and umbilical cord. Human umbilical cord mesenchymal stem cells (hUC-MSC) have advantages over mesenchymal stem cells from other sources: (1) they are isolated from the umbilical cord after the mother has given birth and the cord has been cut, at which point the umbilical cord is discarded as “medical waste”; (2) the collection process is non-invasive for both mother and child; (3) a very large number of cells can be isolated, especially mesenchymal stem cells isolated from umbilical cord tissue; (4) they belong to the category of infant stem cells, so they have higher differentiation and proliferation potential than adult stem cells; (5) the host of the umbilical cord is a newborn baby, so the stem cells are also younger than stem cells in an adult body.
In addition to the above characteristics, a prominent feature of hUC-MSC is their ability to be used in allografts or xenografts without much concern for histocompatibility between the donor and recipient. This characteristic makes hUC-MSC significantly different from MSCs derived from other tissues in treatment. Many research studies have demonstrated this superior property of hUC-MSC (both in vitro and in vivo; in both experimental animals and humans).
One author created a sheet containing hUC-MSCs and applied it to the wounds of experimental mice. They observed that after 10 days, the hUC-MSCs infiltrated and persisted at the wound site in the recipient. Moreover, they also secreted HCG locally (1).
In 2022, Yulin He and colleagues induced liver fibrosis in 6-week-old Wistar rats by intraperitoneal injection of porcine serum at a dose of 0.5 mL twice a week for 11 weeks to create an immune-mediated liver fibrosis model. After 11 weeks, the rats with immune-mediated liver fibrosis were intravenously injected with lipopolysaccharide (LPS) to create an acute-on-chronic liver injury (ACLI) model or a combination of LPS and D-galactosamine (D-GalN) to create an acute-on-chronic liver failure (ACLF) model. Rats with ACLI or ACLF were intravenously injected with 2×10⁶ hUC-MSCs or 0.9% sodium chloride as a control. These rats were euthanized after 1, 2, 4, and 6 weeks (ACLI rats) or 4, 12, and 24 hours (ACLF rats). Blood and liver tissue were collected for biochemical and histological studies. The results showed that the use of hUC-MSCs in rats with ACLI and ACLF led to a significant reduction in serum ALT, AST, TBil, DBil, ALP, ammonia, and PT levels, with ALB gradually returning to normal levels. Inflammatory cell infiltration and collagen fiber deposition in liver tissue were significantly reduced in ACLI rats treated with hUC-MSCs. Inflammatory cell infiltration and apoptosis in the liver tissue of ACLF rats treated with hUC-MSCs were significantly reduced. Compared to rats treated with 0.9% sodium chloride, significantly reduced pro-inflammatory cytokine levels and elevated serum hepatocyte growth factor (HGF) levels were found in ACLF rats treated with hUC-MSCs. Furthermore, Notch, IFN-γ/Stat1, and IL-6/Stat3 signaling pathways were inhibited in ACLI/ACLF rats treated with hUC-MSCs (2).
In 2024, the research group of Sze Piaw Chin published that hUC-MSCs labeled with GFP-Luc2 protein (an oxidative enzyme capable of bioluminescence in the presence of luciferin) were subsequently quantified using flow cytometry (without the need for fluorescence microscopy). After intravenous infusion of the labeled hUC-MSCs into healthy BALB/c mice, the cells were dynamically tracked using bioluminescence imaging (BLI). The results showed that the attachment of GFP-Luc2 to hUC-MSCs not only preserved the characteristics of MSCs but also allowed for direct tracking of the labeled cells in the mouse body. After systemic injection, BLI results showed that hUC-MSCs initially migrated and concentrated in the lungs of healthy BALB/c mice and mainly remained in the lungs for up to 3 days before being cleared from the body. Before sacrificing the mice, plasma biochemical markers remained unchanged except for a significant decrease in C-peptide levels in the hUC-MSC-infused group. Histopathological findings further showed that hUC-MSC infusion did not cause any side effects and was not toxic to lung, liver, and heart tissues (3).
In 2024, the research group of Pham Nguyen Thanh Thuy (Mekostem Stem Cell Bank) conducted intravenous infusion of hUC-MSC-MKS prepared by MEKOSTEM Stem Cell Bank into C57BL/6 mice and monitored their physical condition, biochemical and hematological parameters, and histological images of the liver and spleen for 21 days after infusion. The results showed that the infusion did not cause complications due to embolism or immune responses against the graft; all paraclinical parameters were stable, and there were no pathological changes during the follow-up period (4).
Studies on the safety of allogeneic hUC-MSC infusion in humans have also yielded similar results. Yingqian Zhu and colleagues infused hUC-MSCs into elderly individuals to improve chronic inflammation. The study was conducted using a randomized, double-blind, placebo-controlled method; physical fitness changes were monitored using PCS (physical component scores), and pro-inflammatory cytokine levels were monitored for 6 months. The authors found that hUC-MSC infusion was safe and did not cause complications in the recipients. In the hUC-MSC infusion group, significant improvements in PCS and the levels of pro-inflammatory factors were observed from the first examination after treatment and maintained throughout the follow-up period, with greater changes compared to the placebo group (p = 0.042) (5).
Keklik M and colleagues studied the safety and efficacy of hUC-MSC infusion for the treatment of graft-versus-host disease (GVHD) in 76 patients who developed the syndrome after allogeneic hematopoietic stem cell transplantation. The results confirmed the safety of hUC-MSC infusion as well as the efficacy of hUC-MSC in treating GVHD (6).
Many other studies also show that allogeneic or xenogeneic hUC-MSC infusion does not lead to graft rejection in the recipient, which is a reliable finding.
To explain this superior property of hUC-MSC when infused into allogeneic or xenogeneic recipients, there are two main lines of research: First, demonstrating the changes in HLA expression on hUC-MSCs, especially the role of HLA-G; Second, demonstrating the inhibitory effect of hUC-MSCs on acquired immunity upon allogeneic infusion.
Regarding the first line of research, according to the definition of the International Society for Cell & Gene Therapy (ISCT), mesenchymal stem cells (MSCs) in general from various tissue sources (bone marrow, adipose tissue, umbilical cord, placenta) do not express HLA-DR (only about 1.5% express HLA-DR) (7).
When studying hUC-MSCs, the authors found that hUC-MSCs, like MSCs from other sources, do not express HLA-DR on their surface but differ from other MSC sources in that they express HLA-G. The research group of Dah-Ching Ding demonstrated that HLA-G is a non-classical class I HLA allele that is more highly expressed on hUC-MSCs compared to MSCs from other origins. Flow cytometry analysis showed that 90.8% of hUC-MSCs expressed HLA-G. RT-PCR showed the expression of HLA-G1, HLA-G5, and HLA-G7 in all four hUC-MSC lines (8).
According to the second line of research, the authors demonstrated that hUC-MSCs have an inhibitory effect on acquired immunity.
By culturing lymphocytes in vitro with the addition of hUC-MSCs (co-culture), Ennis’s research group found that hUC-MSCs did not stimulate lymphocyte blast transformation and proliferation. This means that hUC-MSCs do not stimulate the blast transformation and proliferation of allogeneic lymphocytes. In addition, the authors also co-cultured hUC-MSCs with one-way mixed lymphocyte culture (MLC) of two allogeneic individuals, where one population was irradiated to prevent it from reacting to the HLA-DR antigens of the other individual. The results showed that lymphocytes from the non-irradiated individual had a reduced blast transformation response. Furthermore, when hUC-MSCs were introduced into activated T cell lines, the expression of both CD25 and CD45 was significantly reduced. This is in vitro evidence of the immunosuppressive properties of hUC-MSCs on T lymphocytes (9).
Dewi Masyithah Darlan and colleagues demonstrated in vitro that when hUC-MSCs were cultured with peripheral blood mononuclear cells from patients with systemic lupus erythematosus (SLE), hUC-MSCs had an inhibitory effect on the activity of antigen-presenting cells (dendritic cells): significantly reducing CD11c expression on these cells in all groups with the presence of hUC-MSCs. MSCs also significantly reduced the levels of TNF-α, IFN-γ, IL-6 and significantly increased the level of IL-10 in all experimental groups compared to the control group (10).
Recently, in an in vivo experiment, the research group of Jacob P. Nilles performed gene transfer encoding HLA-G into the conjunctiva of mice with sympathetic ophthalmia that occurred after allogeneic bone marrow transplantation (ocular graft vs. host disease). The results showed that chronic inflammatory manifestations in the eyes of mice with graft-versus-host disease improved significantly and had a similar effect to the group treated with cyclosporin A, and were significantly better than the untreated control group (11).
HLA-G is a non-classical class I HLA molecule consisting of four membrane-bound isoforms (HLA-G1, -G2, -G3, and -G4) and three soluble isoforms (HLA-G5, -G6, and -G7). HLA-G is a ligand for several receptors such as LILRB1 and LILRB2, and especially KIR2DL4 on immune cells including NK cells, and plays a role in regulating the activity of immune cells during pregnancy to create maternal-fetal tolerance.
Cell surface HLA-G was first found on cytotrophoblasts and has been shown to maintain maternal-fetal tolerance. In general, HLA-G molecules are involved in inhibiting or suppressing the activity of NK cells, the maturation of CD4+ T lymphocytes and antigen-presenting cells, the apoptosis of CD8+ cytotoxic T lymphocytes (CTLs), and the development of regulatory T cells (12).
In summary, the allograft potential of hUC-MSCs is an important advantage of these cells when used to treat anti-inflammation in diseases related to chronic inflammation, especially in individuals with impaired immune regulation or immunodeficiency, such as the elderly. Although further in-depth research is needed on the mechanism of action of hUC-MSCs, recent studies have confirmed the safety of allogeneic hUC-MSC infusion, especially the absence of graft rejection reactions. The role of hUC-MSCs in general and the high expression of HLA-G on the surface of hUC-MSCs are considered a major topic for research to explain the mechanism of action of hUC-MSCs.
References
- Kyungsook Kim et al.: Human mesenchymal stem cell sheets in xeno-free media for possible allogenic applications.. Sci Rep. 2019.
- Yulin He et. al.:.Human umbilical cord-derived mesenchymal stem cells improve the function of liver in rats with acute-on-chronic liver failure via downregulating Notch and Stat1/Stat3 signaling. Stem Cell Res Ther. 2022 Feb 7;13:65)
- Yulin He Xingrong Guo Tingyu Lan, Jianbo Xia, Jinsong Wang, Bei Li, Chunyan Peng Yue Chen, Xiang Hu Zhongji Meng Dynamic tracking of human umbilical cord mesenchymal stem cells (hUC-MSCs) following intravenous administration in mice model. Sze-Piaw Chin; Marini Marzuki; Lihui Tai et al. Regenerative Therapy Volume 25, March 2024, Pages 273-283).
- Phạm Nguyễn Thanh Thủy, Lê Văn Đông, Mai Văn Điển, Ngô Thị Tuyết Hạnh, Lưu Thị Thu Thảo, Trương Thị Thu Huyền, Phạm Lê Bửu Trúc: Tế bào gốc trung mô mô dây rốn người an toàn khi được ghép trên chuột C57BL/6-Safety of human umbilical cord mesenchymal stem cells in C57BL/6 mice; Tạp chí Khoa học Đại học Mở Thành phố Hồ Chí Minh, 2024, 19(1), 61-70).
- Yingqian Zhu Ce Huang Liang Zheng 6, Qingqing Li, Jianli Ge. Safety and efficacy of umbilical cord tissue-derived mesenchymal stem cells in the treatment of patients with aging frailty: a phase I/II randomized, double-blind, placebo-controlled study. Stem Cell Res Ther. 2024 Apr 29;15:122). doi.
- Muzaffer Keklik, Burak Deveci, Serhat Celik , Kemal Deniz , Zeynep Burcin Gonen, Gokmen Zararsiz, Rabin Saba, Gulsah Akyol, Yusuf Ozkul, Leylagul Kaynar, Ertugrul Keklik, Ali Unal, Mustafa Cetin, Olcay Y Jones: Safety and efficacy of mesenchymal stromal cell therapy for multi-drug-resistant acute and late-acute graft-versus-host disease following allogeneic hematopoietic stem cell transplantation. Ann Hematol. 2023 Jun;102(6): 1537-1547.
- Zyrafete Kuçi, Natascha Piede, Kathrin Vogelsang, Lisa-Marie Pfeffermann, Sibylle Wehner, Emilia Salzmann-Manrique, Miriam Stais, Hermann Kreyenberg, Halvard Bonig, Peter Bader & Selim Kuçi Expression of HLA-DR by mesenchymal stromal cells in the platelet lysate era: an obsolete release criterion for MSCs. Journal of Translational Medicine volume 22, Article number: 39 (2024). (Characteristics of Mesenchymal Stem Cells – New Stars, chapter 2 in Regenerative Medicine or Unrecognized Old Fellows in Autologous Regeneration? edit. By Richard Schäfer 1,*, Hinnak Northoff. Transfus Med Hemother. 2008 May 21;35(3):154–159).
- Dah-Ching Ding, Hsiang-Lan Chou, Tang-Yuan Chu et al.: Characterization of HLA-G and Related Immunosuppressive Effects in Human Umbilical Cord Stroma-Derived Stem Cells. Cell Transplant. 2016.).
- J. Ennis, C. Götherström , K. Le Blanc , J.E. Davies In vitro immunologic properties of human umbilical cord perivascular cells.
- Dewi Masyithah Darlan, Andi Raga, Adi Muradi Muhar, Agung Putra, Iffan Alif: Mesenchymal Stem Cells Suppress Dendritic Cells and Modulate Proinflammatory Milieu Through Interleukin-10 Expression in Peripheral Blood Mononuclear Cells of Human Systemic Lupus Erythematosus. Acta Inform Med. 2023 Mar; 31(1): 20–25.