Nature, 08/05/2025
A phase 1 clinical trial conducted by researchers at Tehran University of Medical Sciences evaluated the safety and feasibility of placenta-derived mesenchymal stem cell (PLMSC) therapy in five patients with secondary progressive multiple sclerosis (SPMS). The results indicated that this therapy is safe and may offer potential clinical benefits.
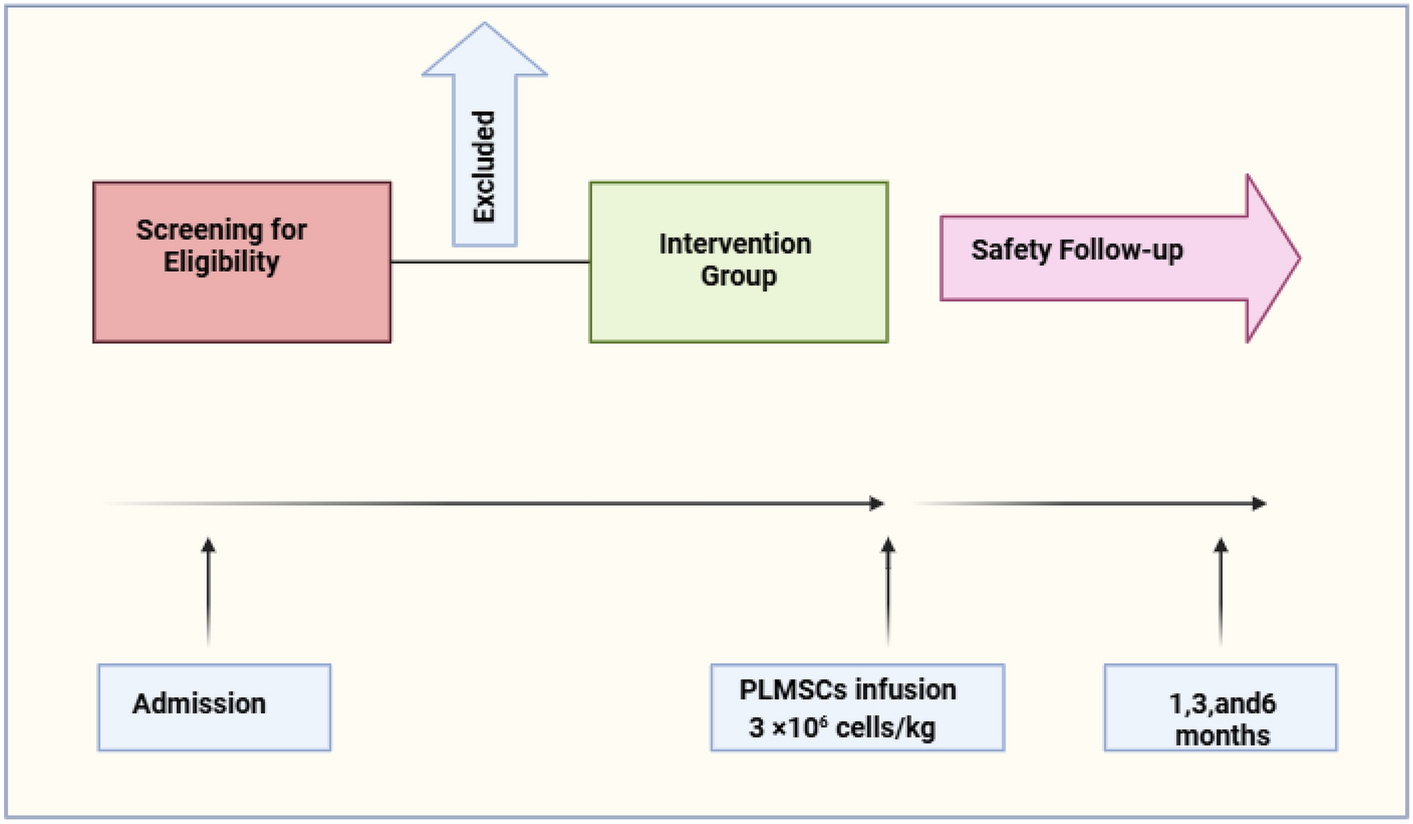
Fig.1 Study design and patient follow-up in the clinical trial
Background
Secondary progressive multiple sclerosis (SPMS) is a degenerative neurological disorder that is difficult to treat, particularly when patients no longer respond to conventional immunosuppressive therapies. Mesenchymal stem cells (MSCs) possess anti-inflammatory, immunomodulatory, and neuroregenerative properties, making them a promising therapeutic approach.
Study Design
- Type: Phase 1, open-label, single-arm clinical trial.
- Participants: 5 SPMS patients aged 25–58, with EDSS scores ranging from 6 to 6.5 (indicating mobility impairment).
- Intervention: A single intravenous dose of PLMSCs, processed under stringent quality control.
- Follow-up duration: 6 months after cell infusion.
Monitored Parameters:
- Neurological evaluation: EDSS (Expanded Disability Status Scale), cognitive and psychological function assessments.
- Neuroimaging:
- DTI (Diffusion Tensor Imaging): to assess white matter integrity.
- fMRI (Functional MRI): to evaluate brain activity and functional connectivity.
- Immunological markers: Plasma cytokines (IL-6, IL-10, TNFα, IL-17), B cell markers (CD19+/CD20+).
Key Results:
- Safety:
- No serious adverse events were reported.
- Two patients experienced mild headaches post-infusion, which resolved spontaneously within hours.
- Clinical Improvement:
- All patients showed significant improvements in EDSS scores (P < 0.0001), indicating a slowdown in disease progression.
- Cognitive function, emotional well-being, and quality of life improved notably, as measured by standardized questionnaires.
- Neuroimaging Changes:
- DTI: Significant reduction in Radial Diffusivity (RD), suggesting improved myelination (P = 0.0186).
- fMRI: Increased functional network connectivity, particularly in the frontal and motor cortex areas.
- Immunological Modulation:
- Elevated anti-inflammatory IL-10 and reduced pro-inflammatory cytokines (IL-6, TNF-α, IL-17) (P < 0.0001).
- Decreased proportions of CD19+ and CD20+ B cells (P = 0.0077), indicating reduced immune activation.
Conclusion:
PLMSC therapy appears to be a safe and feasible intervention for SPMS patients, showing early biological efficacy. Notably, the treatment resulted in immunomodulatory effects, neuroprotection, and functional improvements.
The authors recommend further investigation through a larger, controlled phase 2 clinical trial to confirm these promising findings.
References
This article was translated and summarized from the original publication:
Shokati, A., Nikbakht, M., Sahraian, M.A. et al. Cell therapy with placenta-derived mesenchymal stem cells for secondary progressive multiple sclerosis patients in a phase 1 clinical trial. Sci Rep 15, 16005 (2025). https://doi.org/10.1038/s41598-025-00590-6
Source: Nature
Link: https://www.nature.com/articles/s41598-025-00590-6#citeas






