Stem Cell Reasrch & Therapy, 09/07/2025
Background
Erectile dysfunction (ED) is a common condition in which men are unable to achieve or maintain an erection sufficient for satisfactory sexual intercourse. Approximately 2.5-3% of men develop ED annually, and 20-30% of adult males experience at least one episode during their lifetime. Diabetic ED has a profound impact on psychological well-being, relationships, and quality of life. It is often associated with depression, anxiety, and low self-esteem, which in turn may worsen metabolic control in diabetic patients.
The pathogenesis of ED is multifactorial, involving both modifiable and non-modifiable risk factors such as age, dyslipidemia, hypertension, cardiovascular disease, and physical inactivity. In diabetes, chronic hyperglycemia leads to microvascular injury, neuropathy, and endocrine dysfunction, all contributing to erectile impairment.
Conventional treatment modalities for ED – including oral phosphodiesterase-5 (PDE-5) inhibitors, intracavernosal injections, and vacuum erection devices – may provide temporary symptomatic relief but generally fail to reverse the underlying pathological alterations in the corpora cavernosa. Notably, a subset of patients demonstrates either pharmacotherapeutic resistance or adverse drug reactions.
Low-intensity extracorporeal shock wave therapy (LI-ESWT) has emerged as an innovative physical therapy that utilizes mechanical stimulation to induce local cytokine release and activate endogenous stem and endothelial cells, thus promoting neovascularization and neural regeneration. However, when applied as a monotherapy, LI-ESWT may yield limited and transient benefits, particularly in patients with diabetic ED, where its efficacy often falls short of clinical expectations.
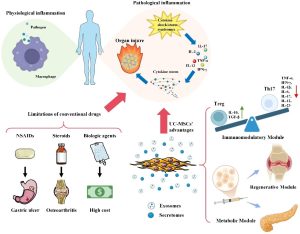
In recent years, mesenchymal stem cells (MSCs) have emerged as a promising area of regenerative medicine due to their multipotent differentiation capabilities, robust secretion of paracrine factors, and low immunogenicity. Placenta-derived MSCs (hPMSCs) are especially attractive due to their easy accessibility, strong regenerative potential, and favorable safety profile. Experimental studies show that MSCs secrete growth factors such as VEGF, HGF and other cytokines that promote angiogenesis, nerve repair, and reduce inflammation – thereby improving erectile function.
Recent investigations have proposed the combined application of MSCs and LI-ESWT as a strategy to optimize the local microenvironment, enhance the survival and functional integration of transplanted cells, and achieve a synergistic therapeutic effect. Building upon these preclinical foundations, contemporary research has increasingly focused on combinatorial regenerative strategies integrating mesenchymal stem cells (MSCs) with low-intensity extracorporeal shock wave therapy (LI-ESWT). This combined approach may address current limitations of standalone therapies by simultaneously targeting multiple pathological mechanisms underlying ED.
Methods
This prospective, randomized, controlled clinical trial aimed to evaluate the efficacy and safety of high-activity placenta-derived mesenchymal stem cells (hPMSCs) combined with low-intensity extracorporeal shock wave therapy (LI-ESWT) in patients with refractory diabetic (type 2 diabetes mellitus) erectile dysfunction (ED).
Human placenta-derived mesenchymal stem cells (hPMSCs) were isolated from placentae obtained from healthy women undergoing full-term cesarean delivery.
A total of 33 eligible patients were enrolled and randomly assigned in a 1:1:1 ratio into three groups: the hPMSCs group (n = 11), the LI-ESWT group (n = 11), and the combined therapy group (H + L, n = 11).
- hPMSCs: The hPMSCs were prepared as a cell suspension with a concentration of 1 × 10⁷ cells/mL. Each patient in the hPMSCs group received a single intracavernosal injection. Following disinfection of the penis and application of a penile constriction band at the base, 1 mL of the cell suspension was injected into the corpora cavernosa (0.5 mL per side). After injection, local compression was applied for 1 min, and the constriction band was maintained for 30 min before removal.
- LI-ESWT: LI-ESWT was performed using a shock wave device targeting both sides of the corpora cavernosa and the penile crura. Low-intensity extracorporeal shockwave therapy was administered using the RENOVA® electromagnetic lithotripter (Direx Group, Wiesbaden, Germany). The treatment parameters were set at an energy density of 0.09 mJ/mm² and a pulse frequency of 120 pulses per minute. For each treatment session, five treatment points were designated (covering the distal, mid, and proximal regions of the penis, as well as the left and right penile crura), with 1,000 shocks delivered at each point, amounting to a total of 5,000 shocks per session.
- hPMSCs + LI-ESWT (H + L): Participants in the combined intervention group underwent a sequential therapeutic protocol: (1) an intracavernous injection of placental mesenchymal stem cells (PMSCs) was administered at baseline, followed by (2) low-intensity extracorporeal shockwave therapy (LI-ESWT) initiated 24 h post-injection. The LI-ESWT regimen consisted of four weekly sessions.
Comprehensive evaluations were conducted at baseline, 1 month, 3 months, and 6 months post-treatment, with adverse events recorded at each follow-up visit. To minimize confounding, all patients discontinued any other ED medications during the study period and for a 2-week washout period prior to intervention.
Results
The baseline IIEF-EF scores were similar across the hPMSCs, LI-ESWT, and H + L groups (p > 0.05). Longitudinal analysis demonstrated an improvement in IIEF-EF scores over time in all treatment arms. Importantly, the H + L group consistently exhibited the most pronounced therapeutic effect at all follow-up time points (1, 3, and 6 months), with significantly higher IIEF-EF scores compared to the single-therapy groups. At 6 months, the combined therapy group achieved a mean IIEF-EF score of 19.8 ± 0.31, which remained significantly higher than the hPMSCs group (17.50 ± 0.53) and the LI-ESWT group (16.67 ± 1.39) (p < 0.05).
Regarding EHS, at baseline and the 1-month follow-up, the proportion of patients with EHS > 2 was similar among the groups (hPMSCs: 18.18%, LI-ESWT: 30%, H + L: 18.18%). Notably, at the 6-month follow-up, the H + L group exhibited a significantly higher proportion of patients with EHS > 2 (70%) compared to the hPMSCs (45.45%) and LI-ESWT (40%) groups (p = 0.045).
In contrast, at the 1-month and 3-month assessments, the success rates recorded as SEP-3 (successful intercourse) did not show significant improvement or intergroup differences (p > 0.05). At 6 months, SEP-3 positivity reached 18.18% in the H + L group, 30% in the LI-ESWT group, and remained at 18.18% in the hPMSCs group, with the differences not achieving statistical significance (p = 0.789). These results suggest that while the combined H + L treatment appears to be more effective in enhancing erection hardness (EHS > 2), its impact on overall sexual performance – reflected by both SEP-2 (penetration success) and SEP-3 (successful intercourse) rates – remains limited and warrants further investigation.
All groups experienced a significant increase in total erection time from baseline to the 6-month follow-up (p < 0.001). At 6 months, the median total erection time was 18.20 min (IQR: 13.35-20.55) in the hPMSCs group, 11.00 min (IQR: 11.00-12.00) in the LI-ESWT group, and 22.20 min (IQR: 15.20-30.25) in the H + L group, with statistically significant differences among groups (χ² = 13.68, p = 0.001). Similarly, effective erection time improved significantly by 6 months to 11.40 min (IQR: 10.75-12.00) in the hPMSCs group, 10.70 min (IQR: 10.33-11.28) in the LI-ESWT group, and 11.90 min (IQR: 11.55-12.35) in the H + L group (χ² = 11.14, p = 0.004).
These findings indicate that over the 6-month observation period, the combined H + L therapy produced a sustained and superior therapeutic effect compared to either monotherapy, suggesting a potential for enhanced and lasting benefits in erectile function recovery.
Conclusion
In conclusion, our study provides preliminary evidence that the combination of high-activity hPMSCs and LI-ESWT is a safe and more effective therapeutic strategy for improving erectile function in patients with diabetic ED compared to either treatment alone. The synergistic enhancement observed in erection duration and hardness suggests that this combined modality may offer a promising avenue for the development of long-term regenerative treatments for ED. Future large-scale, multicenter studies with extended follow-up periods are warranted to validate these findings and to further explore the underlying biological mechanisms.
References
Ji, YH., Zhang, YF., Tan, X. et al. (2025). High-activity placenta-derived mesenchymal stem cells combined with low-intensity extracorporeal shock wave therapy for diabetic erectile dysfunction: a prospective randomized controlled trial. Stem Cell Res Ther 16, 359. https://doi.org/10.1186/s13287-025-04499-9
Source: Stem Cell Reasrch & Therapy
Link: https://rdcu.be/eMuQP