Orphanet Journal of Rare Diseases, 17/10/2025
Background
Cerebral palsy (CP) is the most common cause of functional impairment in young children. CP is a group of conditions that affect movement and posture, arising from damage to the developing central nervous system, typically occurring before birth. Symptoms appear during infancy or the preschool years and range from very mild to severe.
Globally, approximately 3 out of every 1,000 individuals have CP. The annual cost of caring for a patient with cerebral palsy is estimated to be around 87 billion USD for the economies of Australia and the United States. About 70% of CP cases have no identifiable cause, while 20% of cases in children may be associated with prematurity, prenatal trauma, or hypoxic brain injury. In addition, infections and abnormalities occurring during fetal development also contribute to the condition.
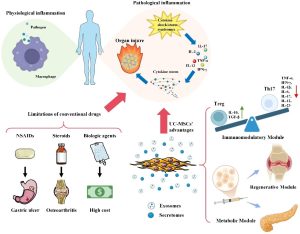
Stem cells are defined as multipotent cells with the capacity for self-renewal and differentiation into various cell lineages. Among stem cell sources, allogeneic umbilical cord blood (UCB) is currently considered a highly valuable source of adult stem cells, containing multiple cell types with diverse therapeutic potential. UCB is derived from mononuclear cells and contains a combination of regulatory T cells, stem cells, and hematopoietic cells. These cells have the ability to modulate the neuroinflammatory environment and are used in the treatment of neurological disorders. In other words, UCB is the most practical option for treating CP due to its demonstrated neuroprotective properties, including anti-inflammatory and anti-apoptotic effects. UCB infusion provides immunological and paracrine signals that enhance cell survival at the injury site, promote progenitor cell proliferation, and stimulate angiogenesis, thereby supporting the treatment of neurological diseases. Additionally, UCB has shown the ability to suppress neuroinflammation by reducing microglial activation and attenuating T-cell responses.
At present, many aspects of UCB-based therapy remain unclear. To establish safe and effective protocols without raising ethical concerns, it is essential to determine the optimal dose, appropriate cell type, and best route of administration for UCB. Considering the importance of stem cells, particularly allogeneic umbilical cord blood, this study was conducted as a systematic review focusing on the safety and therapeutic efficacy of umbilical cord–derived stem cells in patients with cerebral palsy. The objective of the study is to systematically evaluate the safety and effectiveness of allogeneic UCB-derived stem cell therapy in CP patients, thereby providing critical evidence for the global management of cerebral palsy.
Results
In this systematic review, the findings reported from studies evaluating the safety and efficacy of allogeneic umbilical cord–derived stem cell therapy in patients with cerebral palsy were systematically extracted according to the relevant guidelines.
Umbilical cord blood (UCB) is currently one of the best sources of adult stem cells, containing various types of cells with diverse therapeutic potential. Allogeneic UCB has the ability to support the treatment of cerebral palsy. According to the study by Min K. et al. (2013), the concurrent use of recombinant human erythropoietin (rhEPO), a molecule with neurotrophic properties, may enhance the therapeutic effects of UCB. In the same study, UCB treatment improved motor and cognitive impairments in children with cerebral palsy and improved structural and metabolic changes in the brain. Pneumonia and irritability were reported as complications of UCB infusion. However, these are also typical side effects of the immunosuppressant cyclosporine, suggesting that these complications likely arose from cyclosporine rather than from UCB. In contrast to the above findings, other reports have indicated that cyclosporine also exhibits neuroprotective effects similar to EPO, and the combination may provide stronger neuroprotective benefits.
Other adverse effects of stem cell infusion include fever and vomiting. The intrathecal route and treatment in patients ≤ 10 years of age were identified as risk factors associated with these adverse effects. During the first 24 hours after treatment, back pain, headache, and irritability were common adverse effects, mainly associated with the lumbar puncture procedure. Fever was the most frequently observed side effect. One case of arrhythmia occurred during infusion but resolved spontaneously without intervention. Additionally, six patients experienced limb numbness, but the symptoms also resolved on their own.
Many articles demonstrated that stem cell infusion significantly improved motor function. Other studies reported that UCB treatment enhanced muscle strength. Moreover, improved cognitive performance was recorded in one clinical trial. Imaging data from two studies showed structural improvements in white matter after UCB infusion. Consistent with these results, other reports showed that UCB injection significantly improved self-care ability, mobility, and social function; scores on the Cerebral Palsy Quality of Life questionnaire (CP-QOL) in the “family & friends” and “participation” domains were significantly higher than in the control group; and both functional disability level and neurological function showed notable improvements.
Also in the study by Min K. et al. (2013), the treatment group showed increased activation in the bilateral putamen, thalamus, small regions of the bilateral frontal lobes, the right parietal lobe, and the left temporal lobe, whereas the control group displayed increased activity mainly in the bilateral frontal lobes and putamen. Another study reported decreased activity in the white matter of the occipital and temporal lobes bilaterally in the intervention group, accompanied by increased activation in multiple cortical areas within the frontal and parietal lobes. In the control group, brain activity decreased in multiple regions, with only slight increases in some frontal and parietal cortical areas.
It appears that UCB dose or age may influence treatment outcomes after infusion. Patients receiving a high dose showed statistically significant improvements compared with those receiving a low dose. Additionally, greater improvement was observed in older patients with less severe motor impairment, while younger children with severe motor deficits experienced greater cognitive improvement despite minimal motor improvement. Genetic characteristics may also predict the level of responsiveness to stem cell therapy. All selected studies indicated that allogeneic umbilical cord–derived stem cells did not cause any serious or life-threatening complications.
However, in one study, a 25-month-old female patient with quadriplegia due to severe hypoxic brain injury, central gray matter damage, and brainstem injury died 14 weeks after treatment. The child had no head control, severe motor impairment, and required tube feeding due to poor oral motor function, although the parents attempted oral feeding. The patient also had persistent sputum obstruction. Medically, after UCB infusion, the child continued to show neurological improvement until the final assessment (within 3 months). Clinical examination indicated neurological stability at the follow-up in the pediatric neurology department on the day of death. The patient died in her sleep for unknown reasons. After reviewing all data and related events, it was concluded that the death was not related to UCB infusion.
Discussion
Although stem cells derived from umbilical cord blood (UCB) have been introduced as a novel strategy in the treatment of cerebral palsy, a condition that has long-term impacts on patients’ lives, demonstrating their safety and efficacy is essential. Many studies have shown that the use of allogeneic umbilical cord–derived stem cells is safe and effective, and even non-homogeneous UCB infusions may be used to treat CP. The underlying mechanisms that may explain the therapeutic effects of UCB include immunomodulation, secretion of trophic factors, antioxidant metabolism, angiogenic factors, anti-inflammatory, antifibrotic, and anti-apoptotic activities, all of which may enhance the repair of damaged tissues. In mouse models of CP, one preclinical study demonstrated that the prolonged and beneficial effects of allogeneic UCB infusion were due to paracrine actions, promoting the recovery of damaged brain cells and preventing future brain injury. Furthermore, clinical trials have shown that both autologous and allogeneic UCB provide benefits for CP patients.
The reported effects may be related to factors other than stem cells. For example, significant frontal lobe activation observed in experiments using EPO may be attributed to dopaminergic stimulation. In another study, intensive physical exercise may have activated the cerebellum in the untreated control group. One study using UCB showed increased metabolism in the thalamus in the treatment group, which is a promising finding. However, in a previous publication by the same authors, when UCB was not used, perfusion in the thalamus decreased. In another trial, EPO was also administered to the control group in addition to the intervention group; differences in outcomes between the two groups may reflect the effects of UCB on the brain.
It should be emphasized that UCB infusion is generally more appropriate in children and adolescents, as the cells can be collected safely, non-invasively, and with minimal discomfort. Compared with autologous bone marrow stem cell transplantation, the use of allogeneic UCB is less expensive and less time-consuming. The processes of isolation, purification, expansion, characterization, and harvesting of MSCs from bone marrow may take about one month—significantly longer than preparing allogeneic UCB. Recent reports have shown that stem cells may be used to treat neurological disorders. Several studies have demonstrated that allogeneic umbilical cord–derived stem cells have the potential to treat various neurological conditions. Emerging clinical evidence has also indicated the potential use of stem cells, including UCB, for pediatric brain injury. Another study showed that UCB infusion improved gross motor function in patients with severe cerebral palsy.
A non-randomized trial on eight pairs of identical twins (n = 16) showed that one month after intrathecal infusion of allogeneic UCB, gross motor function did not improve significantly in the early months, but showed substantial improvement after six months. The therapeutic effects following UCB infusion were also predicted by genetic factors. The relatively small mean changes in gross motor function observed in several studies may be attributed to baseline characteristics, including participant age. Another study showed that developmental/motor function in children with CP is more promising after 5–7 years of age, and treatment outcomes are better when intervention occurs closer to the time of injury. Additionally, smaller changes in the treatment group may be due to the administration of only a single dose of allogeneic UCB (low-dose or without consecutive dosing).
The most effective method of UCB administration has not yet been determined, but several options exist. Some studies have shown that intravenous or intra-arterial infusion may promote functional development in CP patients. These methods are less invasive than intrathecal injection. However, UCB cells may have difficulty reaching the injury site when administered intravenously/arterially, as the cells may be trapped in other organs or may not cross the blood–brain barrier. Intra-arterial injection is also associated with risks such as microembolism (e.g., blood clots). A case report using a combination of intravenous and intrathecal administration of allogeneic umbilical cord–derived stem cells demonstrated significant improvements in EEG, motor function, and language ability. Although intraventricular injection has also been proposed, not all patients are suitable candidates due to its invasiveness. Four studies showed that intravenous/intra-arterial infusion of allogeneic UCB significantly improved motor function. Another study observed effective outcomes from intravenous UCB infusion, and patients who received a higher HLA-matched dose showed greater motor improvement than those with two HLA mismatches. In summary, the complications associated with stem cells were not severe or life-threatening, and most resolved spontaneously or with supportive care.
Conclusion
According to the studies reviewed, these studies reported that umbilical cord blood–derived stem cells (UCB) have beneficial effects in the improvement and treatment of patients with cerebral palsy. As no serious adverse effects were observed during the use of this therapy in the patients studied, UCB therapy may be considered a potential treatment option for patients with cerebral palsy.
References
Source: Salari, N., Morddarvanjoghi, F., Hosseinian-Far, A. et al. (2025). Safety and efficacy of umbilical cord-derived stem cell therapy for the treatment of cerebral palsy patients: a systematic review. Orphanet J Rare Dis 20, 518.
Link: https://ojrd.biomedcentral.com/articles/10.1186/s13023-025-04029-z