Scientific Reports, 11 August 2025
Scientists have recently published in Scientific Reports a promising combined approach: using human umbilical cord-derived mesenchymal stem cells (UC-MSCs) to treat intrauterine adhesions (IUA) and applying high-resolution ultrasound to monitor endometrial recovery. The results showed that UC-MSCs not only promoted tissue regeneration, but ultrasound also served as an accurate, minimally invasive assessment tool, capable of replacing much of the traditional histological analysis in both research and clinical practice.
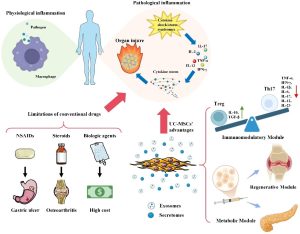
IUA is characterized by adhesions or fibrosis within the uterine cavity caused by endometrial injury, commonly following abortion curettage or gynecological interventions. It can lead to secondary infertility, recurrent miscarriage, and menstrual disorders. Current treatments, such as surgical adhesiolysis, remain limited and carry a high risk of recurrence. Mesenchymal stem cells, particularly those derived from umbilical cord tissue, have emerged as a novel solution thanks to their immunomodulatory, anti-fibrotic, and tissue-regenerative properties.
In this study, researchers used 30 female Sprague–Dawley rats, divided into three groups: normal controls, an IUA model group, and an IUA group treated with UC-MSCs. IUA was induced by mechanical curettage of the endometrium, after which the treatment group received a direct intrauterine injection of 2×10⁷ UC-MSCs. Before the experiment ended, all animals underwent high-resolution ultrasound imaging using the VINNO6LAB system with an 18 MHz transducer, performed before and 14 days after treatment, to measure endometrial thickness and assess mucosal continuity and structure.
Results showed that endometrial thickness in the UC-MSC treatment group reached 0.34 ± 0.06 mm, approaching that of the normal group (0.39 ± 0.05 mm) and significantly higher than in the IUA model group (0.11 ± 0.03 mm, p<0.05). Fibrosis levels decreased from 28.14% in the IUA group to 15.11% in the UC-MSC group. Moreover, endometrial gland structure in the treatment group demonstrated clear restoration, with many glands appearing nearly normal. Notably, ultrasound findings were almost perfectly correlated with histological analysis (r > 0.99, p < 0.0001), indicating high reliability. This suggests that ultrasound could partially replace invasive biopsies in evaluating IUA treatment outcomes.
Demonstrating that ultrasound can accurately assess the effectiveness of UC-MSC therapy opens the door to future non-invasive monitoring for IUA patients. This approach could shorten treatment time, reduce costs, and minimize the need for invasive tissue sampling. Furthermore, the findings strengthen the potential of UC-MSCs as a safe and effective regenerative therapy—not only for IUA but also for other conditions involving endometrial injury.
The study provides strong evidence that combining UC-MSC therapy with ultrasound monitoring could represent a new direction in IUA treatment and management. To bring this approach into clinical practice, larger-scale human trials with longer follow-up periods and comparisons to current standard treatments will be necessary.
References
Guo, S., Li, W., Chen, X., & Liu, M. (2025). Exploring the application value of ultrasound in animal studies of stem cell therapy for intrauterine adhesions. Scientific Reports, 15(1), 1-12.
Source: Scientific Reports
Link: https://www.nature.com/articles/s41598-025-14996-9#citeas