The Scientist, May 14, 2025
Like cancer, placental cells multiply rapidly, invade tissues, and evade destruction by the immune system, but maternal biology somehow keeps them in check.
After centuries of confusion, researchers in the early 1900s were finally beginning to grasp what cancer was and where it came from, correctly identifying certain chemicals and viruses that contributed to the disease. But there were still some theories that didn’t quite hit the mark: Evolutionary biologist John Beard, for example, proposed that cancer cells were trophoblasts—cells that form the outer layer of an early embryo and later become the placenta—that had simply ended up in the wrong place, mistakenly embedding themselves in fetal tissues during development and causing problems later in life.1
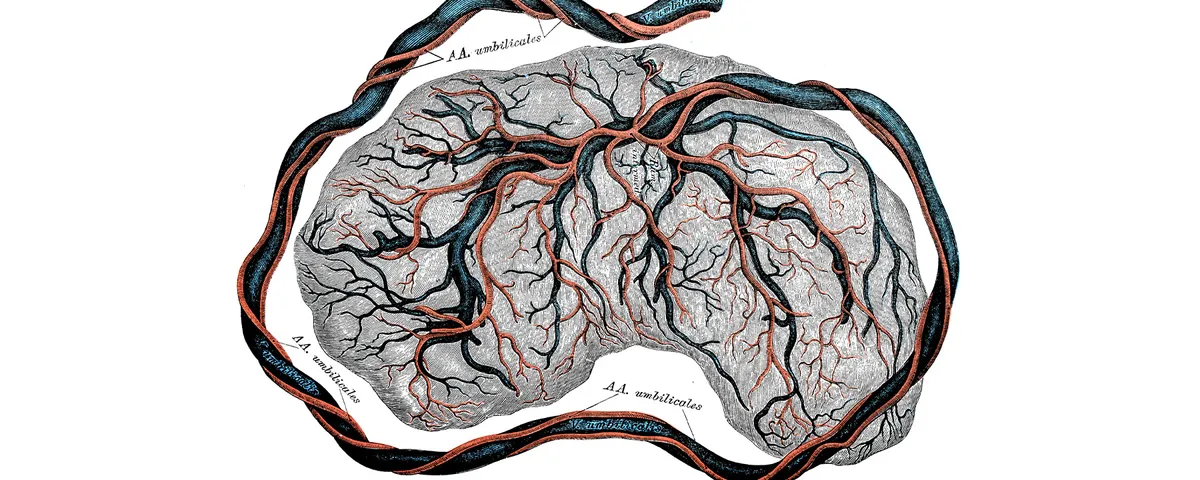
While we now know that tumors don’t originate from trophoblasts, Beard’s theory draws some interesting parallels between placental biology and tumor biology. “The cells from the placenta, they invade into the mother,” said Kshitiz, a cell biologist at the University of Connecticut. “They use many, many similar mechanisms [as cancer], and sometimes they’re innovative mechanisms, too.”
The list of similarities goes on. Placental cells undergo periods of hyperproliferation, supported by upregulation of various growth factors and anti-apoptotic pathways.2 Like tumor cells, they secrete pro-angiogenic factors to promote the growth of blood vessels to gain access to oxygen and nutrients.3 In 2021, researchers at the University of Cambridge sequenced placental tissue samples and were shocked by the level and diversity of genetic mutations, noting that the mutational signatures in the placentas resembled those observed in neuroblastoma or rhabdomyosarcoma.4
“Cancers evade our immune response, they kind of checkmate it by hiding or suppressing the immune response, and thereby surviving, because otherwise cancers would be easily eliminated by our immune system,” said Kshitiz. Like cancer cells, placental cells are also interlopers: While they bear some genetic similarities to the mother, they also carry paternal DNA. Under other circumstances, non-self cells like these would be quickly destroyed by the immune system.
Several studies have indicated that tumors and placentas use similar strategies to manipulate the immune system. Exploring how these immune evasion pathways function in the placenta reveals new targets for disabling these same pathways in cancer cells, rendering them vulnerable to immune attack. In a 2024 paper, for example, a team of researchers at the University of Michigan, led by cancer immunologist Weiping Zou, compared human tumor cells and trophoblast cells using single-cell transcriptomics.5 They found that both populations had elevated expression of B7-H4, an immune checkpoint molecule that inhibits T cell activation.
They then experimentally demonstrated the importance of this molecule in the maternal-fetal interface and in the tumor microenvironment using mouse models. B7-H4 knockout mice were more likely to resorb their fetuses, and they displayed greater T cell infiltration into the placenta than wild type mice. Perhaps even more importantly, in a mouse model of breast cancer, researchers found that pharmacologically reducing B7-H4 levels increased the efficacy of immune checkpoint inhibitors (a group of approved anticancer therapeutics) in reducing tumor progression and prolonging survival.
But this is only one of the ways that placental biology could guide new cancer treatments. In humans, the placenta is highly invasive, sending finger-like projections directly into the mother’s blood. Similarly, malignant cancers must invade the surrounding tissue—the stroma—to spread throughout the body. While the bulk of research has historically focused on the mechanisms used by the placenta or the tumor to infiltrate other tissues, Kshitiz is approaching the problem from the other side: How do the surrounding cells resist invasion?
“Cancer has been considered like a seed in soil,” he said. The characteristics of the seed partly determine how fast it grows, “but it also depends on the soil and how much it allows the cancer to grow.”
Between individual humans, the differences in endometrial or stromal permissiveness may be subtle and are likely influenced by environmental as well as genetic factors, which makes it difficult to determine exactly which genes are involved. Differences across species, however, are much more pronounced. Primates and rodents have highly invasive placentas (or highly permissive endometria), but other mammals are better at setting boundaries: Dogs and cats have intermediately invasive placentas, while horses and cows experience minimal invasion.6
Kshitiz and his colleagues compared the genetics of several species across this spectrum, and identified hundreds of genes that correlated with degree of invasion, as well as a few transcription factors that seemed especially important for regulating these genes.7 Then, they used 3D tissue models populated with human cells to study how knockout of these transcription factors affected permissiveness to invasion. They found that knockout of either GATA2 or TFDP1 transcription factors in human endometrial fibroblasts significantly increased their resistance to invasion by trophoblasts, akin to an animal with a minimally invasive placenta, like a cow. Importantly, knockout of these same factors in skin cells increased their ability to resist invasion by malignant melanoma cells.
“Basically, if we can make humans cow-like then they will be able to resist invasion,” said Kshitiz. “The problem is, of course, we do not want to make the whole person like a cow, but we can locally become cow-like—around the cancer. So, we are now developing a gene therapy which will involve taking a biopsy of the patient’s [healthy] cells and making them cow-like by changing certain genes and then put them back near the cancer.”
In this way, careful examination of the maternal-fetal interface and the molecular cascades that govern cell invasion, immune evasion, and other processes that benefit the fetus may lead to new strategies that can disable these same processes in cancers.
References
- Moss RW. The life and times of John Beard, DSc (1858-1924). Integr Cancer Ther. 2008;7(4):229-251.
- Costanzo V, et al. Exploring the links between cancer and placenta development.Open Biol. 2018;8(6):180081.
- Metzler VM, et al. Androgen dependent mechanisms of pro-angiogenic networks in placental and tumor development. Placenta. 2017;56:79-85.
- Coorens THH, et al. Inherent mosaicism and extensive mutation of human placentas.Nature. 2021;592(7852):80-85.
- Yu J, et al. Progestogen-driven B7-H4 contributes to onco-fetal immune tolerance.Cell. 2024;187(17):4713-4732.e19.
- PrabhuDas M, et al. Immune mechanisms at the maternal-fetal interface: Perspectives and challenges. Nat Immunol. 2015;16(4):328-334.
- Suhail Y, et al. Tracing the cis-regulatory changes underlying the endometrial control of placental invasion. Proc Natl Acad Sci. 2022;119(6):e2111256119.
Source: The Scientist
Link: https://www.the-scientist.com/optimizing-in-vitro-production-of-monocyte-derived-dendritic-cells-and-macrophages-72550








