Stem Cell Research & Therapy, 17/11/25
Background
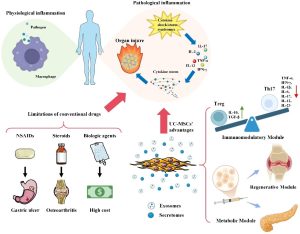
Although the pathogenesis of rheumatoid arthritis (RA) is not yet fully understood, updated studies have suggested that various pro-inflammatory cytokines and immune cells play significant roles in its development and progression. Despite great medical advances in RA therapeutic drugs, only a minority of patients can achieve disease remission and persistent remission off therapy.
Numerous clinical studies have employed allogeneic mesenchymal stem cells (MSCs), primarily derived from adult bone marrow, adipose tissue or umbilical cord (UC), for treating various clinical diseases. The unique anti-inflammatory and immunosuppressive properties of MSCs have led to their widespread application in autoimmune diseases, garnering widespread recognition for their efficacy and short-term safety. Over the past decade, MSCs transplantation (MSCT) has been attempted in systemic lupus erythematosus, Sjogren’s syndrome, systemic sclerosis, graft-versus-host disease, and dermatomyositis/polymyositis, demonstrating satisfactory clinical safety. Theoretically, long-term effects after MSCT may include potential immunosuppression, infection and tumorigenesis. However, to date, there have been no reports on the long-term safety and efficacy of MSCT for the treatment of patients with rheumatoid arthritis.
In the current study, MSCs monotherapy and MSCs combined with IFN-γ treatment were conducted in the two phase 1/2 randomised, double-blind 48-week studies.MSCs significantly improved the signs and symptoms of RA, and the physical function and health status of patients with moderately to severely active RA responded poorly to regular clinical treatments. In addition, MSCs in combination with IFN-γ demonstrated superiority to MSCs therapy alone. Patients who participated in the core double-blind randomised clinical trials (RCTs) could participate the following long-term extension (LTE) study after signing the informed consent form (ICF).
Methods
- Patient population
The core RCTs enrolled adults with active RA who had an inadequate response to or were intolerant of conventional treatments, including csDMARDs, NSAIDs, bDMARDs, and steroids. Patients who completed the 48-week follow-up period were eligible for continued observation in the long-term extension (LTE) study.
- Study design
In the core RCTs, patients with an inadequate response to conventional treatments were randomized, depending on the study, to receive either a single intravenous dose of MSCs (1 × 10⁶ cells/kg) or MSCs (1 × 10⁶ cells/kg) combined with intramuscular IFN-γ (1 million IU). The source and preparation of MSCs, derived from a single donor, were consistent across all participants. Patients who completed the core RCTs and consented to participate in the LTE study were maintained on a standardized medication tapering protocol. Tapering protocols followed our published criteria, requiring sustained DAS28 < 3.2 for ≥ 12 weeks prior to each step. If the status of a subject continued to improve, a withdrawal schedule was used to taper off the conventional drug treatment regimen in the following order: glucocorticoids, NSAIDs then DMARDs. All treatment modifications were approved by the rheumatologist in charge.
- Clinical response
Efficacy assessments included the Disease Activity Score 28 (DAS28) < 2.6 (indicating remission) and ≤ 3.2 (indicating low disease activity), American College of Rheumatology (ACR) 20/50/70 responses, and the Health Assessment Questionnaire-Disability Index (HAQ-DI). These assessments were conducted in compliance with the European Alliance of Associations for Rheumatology (EULAR) recommendations for reporting clinical trial extension studies in rheumatology.
- Statistical analysis
The safety population included all patients who received MSC transplantation, analyzed in two groups: (1) MSC monotherapy and (2) MSC + IFN-γ. Baseline safety values were defined as the latest measurements before infusion. AEs were summarized by total counts and exposure-adjusted event rates (per 100 patient-years). Follow-up duration was measured from infusion to the last safety assessment.
Efficacy was evaluated in all randomised subjects receiving MSCs transplantation who completed ≥ 5 years of follow-up (Fig. 1). Discontinued patients or those who did not enter the LTE phase were classified as non-responders, while the completer analysis included only patients with data available at each analysis time point.
Statistical analyses used t-tests or Mann-Whitney U tests, and ANOVA when comparing > 2 groups. Changes in continuous variables (e.g., DAS28-ESR, HAQ-DI) were evaluated using mixed-effect models. Remission duration, low disease activity, and ACR20/50/70 responses were assessed with Kaplan-Meier analysis. Trends were evaluated using χ² tests, and treatment adjustments with Fisher’s exact test. Significance was set at p < 0.05.
Results
- Patient disposition
A total of 110 RA patients were randomized to the core RCTs and enrolled in the LTE study, and 97 (88.2%) completed the five-year LTE study. Overall, 13 (11.8% of those randomised initially) patients discontinued the study during the LTE study: 7 (6.4%) due to lack of efficacy, 6 (5.5%) due to AEs. Two patients who discontinued study from the MSCs combined with IFN-γ treatment group not only developed new-onset autoimmune disorders but also failed to achieve an ACR20 response. Among 97 patients who completed the 5-year follow-up, 69 patients received MSCs monotherapy, whereas 28 patients were treated with a combination of MSCs and IFN-γ. The maximum follow-up duration was seven years, with a mean follow-up period of six years (range: 5-7 years). Demographics and clinical characteristics were well-balanced across MSC treatment groups and between study completers and dropouts.
Safety
- Adverse events
A total of 223 adverse events (AEs) were recorded during the follow-up period. The exposure-adjusted event rate (ER) per 100 patient-years was 36.17 in the MSC monotherapy group and 35.86 in the MSC + IFN-γ group. The most frequently reported AEs were decreased lymphocyte count and coronavirus disease 2019. Most lymphocyte reductions occurred within four weeks post-treatment, no grade ≥ 3 events were observed, and all resolved spontaneously by week 8-12. No significant abnormalities were detected in routine bloodwork, liver/kidney function tests, chest radiographs, urinalysis, or electrocardiography.
- Serious adverse events
Serious adverse events (SAEs) were reported in eight patients (7.3%), with exposure-adjusted rates of 2.47/100 PY in the MSC monotherapy group and 2.31/100 PY in the MSC + IFN-γ group. The most common SAEs were autoimmune disorders and infections. The exposure-adjusted rates of autoimmune disorders were 0.45/100 PY in the MSC group and 1.16/100 PY in the MSC + IFN-γ group, including new-onset systemic lupus erythematosus (SLE) and Sjögren’s syndrome.
Clinical response
- Disease activity
Efficacy assessments demonstrated that MSCs combined with IFN-γ is a more effective treatment than MSCs monotherapy for active RA with both clinical and functional improvements observed in many patients.
In the RCT period, ACR20 response rates and DAS28 LDA (≤ 3.2) rates were higher in RA patients treated with MSCs combined with IFN-γ than in patients with MSCs monotherapy (100% vs. 50.7%, 39.3% vs. 8.7%, respectively), and the rates remained stable up to year five of the LTE study (89.3% vs. 44.9%, 42.9% vs. 8.7%, respectively).
For the more stringent responses, namely ACR50/70 and DAS28 remission (< 2.6), at year three and year five of LTE study, a significant difference was also observed with DAS28 remission rates (25% vs. 1.4% and 25% vs. 2.9%, respectively) between the two MSCs administration regimens. The decreases of DAS28 and HAQ-DI scores also stabilized from year one of RCTs to year five of LTE study.
Furthermore, analysis of the durations of ACR20/50/70, DAS28 remission, and DAS28 LDA revealed that, as of the last follow-up visit, clinical efficacy stabilized in both MSCs monotherapy and MSCs combined with IFN-γ treatment group, which demonstrated a remarkable result given the preceding treatment history of this pooled population.
The change in disease activity clusters of the two MSCs groups remained relatively stable throughout the LTE study. Compared with that in the MSCs monotherapy group, the improvement in disease activity in the MSCs combined with IFN-γ treatment group was much more obvious that most patients had moderate or low disease activity, and a few patients experienced remission.
- Medication regimens
Consistent with the observed clinical efficacy, medication regimens adjustments revealed that the number of patients using biological DMARDs (bDMARDs) and prednisone decreased in both of MSCs groups while maintaining anchor therapy with csDMARDs during the LTE study. Notably, compared with the MSCs monotherapy group, the MSCs combined with IFN-γ treatment group exhibited a greater reduction in prednisone use. Notably, sustained drug-free remission was observed in one patient in the MSCs combined with IFN-γ treatment group, with remission achieved within the first follow-up year and maintained through the fifth year.
Conclusions
This LTE study confirmed that MSCs monotherapy provides a sustained favorable safety and efficacy profile, and a combination therapeutic strategy of MSCs plus IFN-γ greatly improved the clinical efficacy of MSC-based therapy in patients with active RA. Rates of TEAEs, SAEs, infections, and malignancies remained low, with no cases of GVHD or death. Laboratory abnormalities were mild, with transient lymphocyte reduction consistent with MSC immunomodulation. Although four patients developed new autoimmune disorders associated with poor therapeutic response MSC therapy overall did not increase immunosuppression-related risks.
Clinical responses were achieved early and sustained throughout the 5-year follow-up, with MSC + IFN-γ outperforming MSC alone across multiple measures, including DAS28, ACR20/50/70, and reductions in prednisone and bDMARD use. Despite limitations such as single-center design, moderate sample size, and lack of radiographic evaluation, the findings support the durability and safety of MSC-based therapy.
In conclusion, MSCs combined with IFN-γ provide meaningful, long-term clinical benefit and represent a promising therapeutic option for RA patients who respond inadequately to conventional treatments.
References
Yang, Y., He, X., Yao, M. et al. (2025). Mesenchymal stem cells combined with IFN-γ treatment versus mesenchymal stem cells monotherapy: safety and efficacy over five years extension follow-up. Stem Cell Res Ther 16, 642.
https://doi.org/10.1186/s13287-025-04772-x
Source: Stem Cell Research & Therapy
Link: https://rdcu.be/eQFIb