International Journal of Molecular Sciences, 20/08/2025
Background
Despite remarkable advancements in medical science, diabetes, particularly type 1 diabetes (T1D), continues to pose significant health challenges. Individuals with T1D are highly susceptible to a variety of complications, with vascular disorders being among the most severe and life-threatening. Over time, these abnormalities lead to devastating clinical outcomes such as nephropathy (kidney disease), retinopathy (eye disease), neuropathy (nerve damage), and cardiovascular diseases including coronary artery disease.
A central player in the development of these complications is endothelial dysfunction, which is a hallmark of diabetes. The endothelium, a thin layer of cells lining blood vessels, plays a critical role in maintaining vascular homeostasis by regulating blood flow, inflammation, and coagulation. In diabetes, chronic hyperglycemia (elevated blood glucose levels) and oxidative stress disrupt endothelial function, leading to vascular injury. Elevated glucose levels trigger the overproduction of reactive oxygen species (ROS), such as hydrogen peroxide (H₂O₂), within endothelial cells.
ROS are highly reactive molecules that cause oxidative damage to cellular components, including lipids, proteins, and DNA. This oxidative stress impairs the endothelial lining, reducing its ability to produce nitric oxide (NO), a key molecule that promotes vasodilation and maintains vascular health. As a result, the blood vessels become more prone to inflammation, thrombosis, and atherosclerosis, contributing to the progression of diabetic complications.
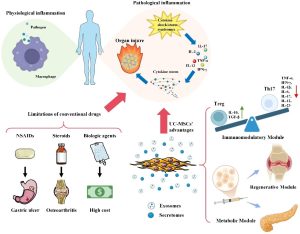
In recent years, stem cell biology has emerged as a groundbreaking field in therapeutic and regenerative medicine. Stem cells, with their unique ability to self-renew and differentiate into various cell types, offer immense potential for treating a wide range of diseases, including cardiovascular diseases, immunological disorders, cancer, diabetes, and organ injuries. Among the various types of stem cells, mesenchymal stem cells (MSCs) have garnered significant attention due to their versatility and therapeutic properties. MSCs are multipotent cells that can be isolated from adult tissues such as adipose tissue, bone marrow, umbilical cord, dental pulp, and the placenta. Their ability to migrate to sites of injury and modulate immune responses makes them attractive candidates for treating metabolic and immune-related diseases.
Human term placental MSCs were isolated from distinct anatomical regions, including decidua basalis MSCs (DBMSCs), decidua parietalis MSCs (DPMSCs), and chorionic villus MSCs (CVMSCs), collectively referred to as placenta-derived MSCs (pMSCs). These cells demonstrated the capacity to differentiate into mesenchymal lineages and secrete a variety of cytokines, growth factors, and immunomodulatory molecules. pMSCs have been shown to protect endothelial cells from inflammatory activation and oxidative stress, particularly H₂O₂-induced damage.
These findings highlight the therapeutic potential of pMSCs in mitigating endothelial dysfunction, making them a compelling candidate for further investigation in animal models of diabetes-induced vascular complications.
Methods
Isolation and Culture of pMSCs
Human term placentas (38-40 weeks) were collected from healthy donors with informed consent. pMSCs were isolated from the decidua basalis region, cultured in DMEM-F12 supplemented with 10% fetal bovine serum and antibiotics, and maintained at 37°C with 5% CO₂. Only cultures with cell viability above 90% were used. Cells from twenty placentas were pooled to minimize donor variability.
Induction of Diabetes in Animal Models
Twenty-four male C57BL/6 mice (8 weeks old) were divided into control and diabetic groups. Type 1 diabetes was induced by intraperitoneal injections of streptozotocin (STZ, 40 mg/kg/day) for five consecutive days. Mice with blood glucose > 150 mg/dL on two consecutive readings were considered diabetic. On day 51, kidney, heart, and retinal tissues were collected for histological analysis.
pMSCs injections
Mice were assigned to four groups: control, pMSC only, diabetic, and diabetic + pMSC (n = 6 per group). Diabetic + pMSC mice received 1 × 106 pMSCs in 0.2 mL PBS by intraperitoneal injection, while diabetic controls received PBS alone.
Glucose Tolerance Test (GTT)
After a 14 h fast, mice received 2 mg glucose/g body weight intraperitoneally. Blood glucose was measured at 0, 15, 30, 45, 60, 90, and 120 mins.
Insulin Tolerance Test (ITT)
After a 2 h fast, mice received insulin (0.75 U/kg, i.p.), and blood glucose levels were recorded over 120 min.
Histological Staining and Analysis
Kidney, heart, and retinal tissues were fixed in 4% paraformaldehyde, embedded in paraffin, and sectioned at 4 µm thickness. Slides were stained with Hematoxylin & Eosin and Picrosirius Red, then measured glomerular area, retinal layer thickness, and collagen proportionate area (CPA).
Results
pMSC treatment did not significantly improve glucose regulation or insulin sensitivity, indicating no direct effect on systemic glucose metabolism.
Histological analysis revealed a significant reduction in collagen deposition within renal tissues of pMSC-treated diabetic mice compared with untreated diabetic controls. This suggests that pMSCs alleviate renal fibrosis and help preserve kidney architecture, indicating a protective effect against diabetic nephropathy.
pMSC treatment significantly restored total retinal thickness and its sublayers (OPL, ONL, and photoreceptor layers) compared to untreated diabetic mice. These findings indicate that pMSCs protect against retinal degeneration and may prevent diabetic retinopathy progression.
Conclusions
This study demonstrated that systemic administration of placenta-derived mesenchymal stem cells (pMSCs) did not improve insulin sensitivity in STZ-induced diabetic mice. However, pMSCs effectively prevented the progression of diabetes-associated microvascular complications, including nephropathy, retinopathy, and cardiac vascular injury. These findings highlight the therapeutic potential of pMSCs as a promising strategy for preventing and reversing diabetes-induced vascular complications. Further investigations are required to clarify the underlying mechanisms before clinical translation can be achieved.
References
Basmaeil, Y., Bakillah, A., Al Subayyil, A. M., Bin Kulayb, H. N., AlRodayyan, M. A., Al Otaibi, A., Mubarak, S. A. S., Alamri, H. S., Kondkar, A. A., Iqbal, J., & Khatlani, T. (2025). Placenta-Derived Mesenchymal Stem Cells (pMSCs) Reverse Diabetes-Associated Endothelial Complications in a Preclinical Animal Model. International Journal of Molecular Sciences, 26(16), 8057.
https://doi.org/10.3390/ijms26168057
Source: International Journal of Molecular Sciences
Link: https://www.mdpi.com/3457600