Stem Cell Reasrch & Therapy, 14/10/2025
Background
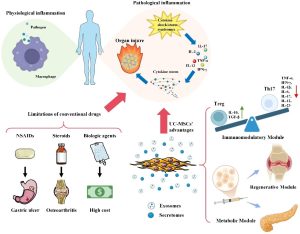
Meniscus injury (MI) is a common condition, particularly affecting athletes and active individuals. While meniscectomy is the primary treatment option for MI, this approach may accelerate the development of osteoarthritis and other degenerative joint diseases, and its therapeutic efficacy remains controversial. Managing MI is challenging due to the meniscus’s limited blood supply, which hinders healing and recovery. Given the limitations of traditional therapeutic strategies, novel strategies are urgently required.
Mesenchymal stem cells (MSCs) have emerged as a promising alternative for promoting meniscal regeneration. This study focused on the secretome, also known as the conditioned medium (CM), derived from human placenta-derived MSCs (pcMSCs). The pcMSC secretome is known for its strong immunomodulatory and regenerative properties. Compared to MSCs, the secretome can easily penetrate smaller wounds and exert lasting effects in vivo. Endogenous meniscus progenitor cells (MPCs) play a crucial role in meniscus regeneration. However, the effect of MSCs/secretome on activating endogenous MPCs to ameliorate MI and the underlying mechanisms remain unclear.
Methods
The pcMSC secretome was collected from pcMSCs cultured in serum-free MCDB201 medium. The secretome was harvested through centrifugation and filtering, and stored at −80°C, ensuring only one freeze–thaw cycle to prevent degradation of paracrine factors.
Cellular MI Model (in vitro): A cellular injury model was established by challenging mouse MPCs with H2O2 (100 or 200 µM) to induce apoptosis and senescence.
Murine MI Model (in vivo): 7-week-old male C57BL/6 mice were subjected to MI induction via destabilization of the medial meniscus (DMM) surgery. Mice were pre-trained for 2 weeks for behavioral tests. Functional motor activity was evaluated weekly until week 11 through gait analysis and rotarod tests.
Protein expression was analyzed using Western blotting, flow cytometry (to assess markers like CD44, Sca-1, CD140, CD34, CD105), and immunohistochemistry staining. Cell viability was assessed using the WST assay.
Tissue samples were subjected to histological analysis including hematoxylin and eosin (H&E) and safranin-O (SO) staining to evaluate tissue structure and proteoglycan content. Masson’s trichrome staining was also used to assess collagen fiber distribution. Immunofluorescence staining was performed using markers such as Ki67 (proliferation), Gli-1 (MPC marker), and TNF-α (inflammation).
Key secretome factors were identified using cytokine arrays (Human Cytokine Arrays C5), utilizing 700 µg/mL of the secretome. Exosomal miRNA analysis was performed using ultracentrifugation for exosome isolation, followed by RNA extraction, library preparation (QIAseq miRNA Library Kit), and sequencing (Illumina/Novaseq 6000), with data accessed via GEO (accession number: GSE247568). TargetScan was used to predict miRNA target genes.
Results
The pcMSC secretome significantly mitigated MI in both cellular and mouse models. The pcMSC secretome repairs mechanically induced meniscus injury in mice by activating the proliferation and suppressing the apoptosis of endogenous meniscus progenitor cells. Secretome treatment markedly increased the expression of both Gli-1 and Ki67 proteins in the meniscus tissue of mice with DMM-induced MI. Additionally, the pcMSC secretome significantly reduced the levels of tumor necrosis factor-α (TNF-α), supporting its role in immunomodulation and meniscus repair.
The regenerative effects are mediated through the paracrine factors and exosomal miRNAs present within the pcMSC secretome. The identified factors involved in the regulate endogenous stem cell activation (SUFU and RUNX2), anti-inflammatory responses (MCP1 and MCP3), anti-cartilage matrix degradation (TIMP1, TIMP2, and mTOR), and apoptosis (Caspase-3).
Conclusion
This is the first study using both in vitro model of H2O2-challenged MPCs and in vivo model of mechanically DMM-induced MI to demonstrate the therapeutic efficacy of the human pcMSC secretome through activating the meniscus progenitor cells in meniscus regeneration.
The essential factors present within the secretome are growth factors and exosomal miRNAs; these factors regulate:
- The activation of endogenous MPCs (promoting MPC proliferation and suppressing apoptosis).
- The immunomodulation of injured tissue (by alleviating inflammation).
- The reconstruction of the ECM (by preventing cartilage matrix degradation and promoting cell migration).
Overall, our findings may guide the development of effective stem cell therapies for patients with exercise-induced meniscus injuries.
References
Chen, WH., Lai, WY., Le, DC. et al. (2025). Secretome from human placenta-derived mesenchymal stem cells repairs mechanically induced meniscus injury in mice by activating the proliferation and suppressing the apoptosis of endogenous meniscus progenitor cells. Stem Cell Res Ther 16, 565.
https://doi.org/10.1186/s13287-025-04688-6
Source: Stem Cell Reasrch & Therapy
Link: https://rdcu.be/eL6e8