Stem Cell Research & Therapy, 15/10/2025
Introduction
According to the World Heart Report 2023, cardiovascular diseases (CVDs) cause approximately 18.6 million deaths each year, accounting for 32% of global mortality. Myocardial infarction (MI) and atherosclerosis (AS) are among the leading causes of death worldwide.
Despite the efficacy of contemporary therapeutic interventions, including coronary artery bypass grafting and anticoagulant administration, these approaches fail to restore function in myocardial or vascular tissues, thereby predisposing patients to persistent heart failure risks.
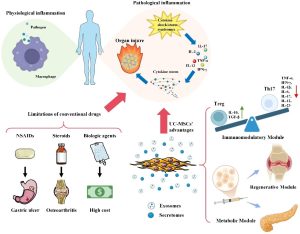
As a type of cell with self-renewal and multilineage differentiation potential, stem cells have unique advantages in repairing damaged tissues. Studies have shown that MSCs can significantly promote angiogenesis and tissue repair by secreting exosomes that release bioactive molecules such as vascular endothelial growth factor (VEGF) and hepatocyte growth factor (HGF). In addition, induced pluripotent stem cells (iPSCs) also provide new possibilities for the precision treatment of CVDs owing to their high plasticity and potential for personalized therapy.
Action pathways of stem cell therapy
- Paracrine effect: Release VEGF, FGF, and other growth factor through exosomes, which promote the proliferation of vascular endothelial cells and angiogenesis in ischemic areas. In addition, cytokines and chemokines can regulate cell apoptosis and fibrosis.
- Direct differentiation: iPSCs can differentiate into functional cardiomyocytes to replace the damaged myocardium.
- Immune regulation: Inhibition of T-cell activation and reduction of pro-inflammatory factors such as TNF-α and IL-6, thereby decreasing inflammatory responses.
- Homing effect: Ability of stem cells to migrate to the site of damaged tissues.
- Intercellular material transfer: Transfer organelles, such as mitochondria, to these cells to provides energy support for damaged cells and promotes their survival and functional recovery.
- Antioxidant and anti-apoptotic effects: Secrete antioxidant factors to remove reactive oxygen species in the body, and reduce oxidative stress; secrete anti-apoptotic factors to prevent cell death and protect damaged tissues.
Application of stem cell therapy in myocardial infarction
MI results from acute coronary artery occlusion that causes severe ischemia and oxygen deprivation, leading to rapid cardiomyocyte loss through necrosis, apoptosis, and regulated cell death such as necroptosis and ferroptosis. Subsequently, fibroblasts differentiate into myofibroblasts that deposit extracellular matrix proteins, resulting in scar formation which preserves structural integrity but impairs electromechanical coupling and diastolic compliance These processes collectively lead to progressive ventricular dysfunction and ultimately heart failure.
Application of stem cell therapy:
- Paracrine effects of MSCs: Secreted factors such as VEGF and HGF stimulate angiogenesis, enhance endothelial survival, and reduce cardiomyocyte apoptosis.
- Exosome-mediated anti-fibrotic effects: Cardiac stem cell release exosomes enriched with microRNAs (e.g., miR-146a, miR-21) that regulate inflammatory signaling and suppress fibrosis.
- iPSC-derived cardiomyocyte replacement: iPSC-derived cardiomyocytes provide a direct source of contractile cells capable of integrating into host myocardium and replacing lost cardiomyocytes after infarction.
Application of stem cell therapy in atherosclerosis
AS is initiated by endothelial dysfunction, lipid accumulation, and macrophage infiltration, leading to foam cell formation and chronic inflammation. Progressive plaque development eventually destabilizes the vascular wall, predisposing to rupture and thrombosis.
Application of stem cell therapy:
- Immunomodulation by MSCs: MSCs regulate immune homeostasis by promoting macrophage polarization toward the M2 anti-inflammatory phenotype. This shift reduces the release of pro-inflammatory cytokines such as TNF-α and IL-6, thereby attenuating vascular inflammation.
- Endothelial repair via endothelial progenitor cells and iPSC-derived endothelial cells: These cells play a pivotal role in vascular repair by accelerating re-endothelialization, promoting neovascularization, and restoring barrier integrity.
- Plaque stabilization: Enhance collagen deposition in fibrous caps and limit necrotic core expansion, thereby improving plaque stability.
Challenges and future direction
Challenges:
- Cell survival after transplantation is low
- Immune rejection
- Ectopic differentiation and tumorigenesis
- Lack of standardized quality control in cell manufacturing
- Long-term safety verification
Future direction:
- Advances in biomaterials and 3D bioprinting may improve cell survival and integration
- Gene-editing technologies enable precise lineage commitment and reduce tumorigenic risk
- Exosome-based, cell-free therapies enriched with cardioprotective microRNAs represent a particularly promising alternative to direct cell transplantation
- Integration of single-cell omics, artificial intelligence, and precision medicine is expected to accelerate personalized approaches
References
Wan, X., Qian, C., Liu, S., Xu, Y., Yuan, J., Zhang, X., & Li, X. (2025). Stem cell therapy for myocardial infarction and atherosclerosis: mechanisms, challenges, and future directions. Stem Cell Research & Therapy, 16(1). https://doi.org/10.1186/s13287-025-04678-8
Source: Stem Cell Research & Therapy
Link: https://link.springer.com/article/10.1186/s13287-025-04678-8