Parent’s Guide to Cord Blood, March 2021
Frances Verter, PhD
Sometimes babies are born with a hernia, which includes any situation where organs protrude through a weak spot in the surrounding muscle or connective tissue. Mild hernias are fairly common but more serious hernias require surgical intervention. The most common hernia in babies is an Umbilical Hernia, which is a bulge under the belly button that occurs in 10-15% of babies and usually closes on its own by the time the child is a few years old1.
A Congenital Diaphragmatic Hernia (CDH) only occurs once in 2500 births but is a serious condition2,3. In CDH, a hole in the diaphragm allows some of the baby’s intestines, and maybe the liver too, to move into the chest cavity. If this is not diagnosed during a prenatal ultrasound, it leads to a crisis at birth, when the baby needs to start breathing through its lungs, but the lungs are compressed by the intestines in the chest cavity. Early intervention is critical.
Babies born with CDH need surgery to move their intestines back down to the abdominal cavity and close the hole in the diaphragm so that they can breathe properly. These babies can be at risk for brain injury due to a lack of oxygen in the blood. One clinical trial NCT03526588 launched in 2018 at the University of Texas is attempting to ameliorate neurologic injury in these infants by giving them a few small infusions of their own umbilical cord blood stem cells.
Another serious hernia is Gastroschisis, where a hole in the abdominal wall allows some of the baby’s intestines to escape outside its body4,5. This only occurs once in about 5,000 births but requires surgical intervention. In utero, the portion of the intestine that is outside the body, floating in the amniotic fluid, becomes swollen and may become twisted. At birth, surgeons usually cannot just push this swollen intestine back into the abdominal cavity. The repair may have to be performed in stages, and the baby may require a patch to close the gap in the abdominal wall.
A team in Quito, Ecuador, has developed and published a surgical technique where the baby’s own umbilical cord is used to form a patch during surgery to correct Gastroschisis6-8. Surgeon Edwin Ocaña manually introduces the exposed abdominal contents into the abdominal cavity. He then takes a section of umbilical cord, ligates the blood vessels, and filets the cord lengthwise to expose the interior Wharton’s Jelly without disrupting the blood vessels. This filet of cord becomes a patch which is placed with the Wharton’s Jelly against the defect, and is further protected with a hydrocolloid patch on top. The tissue patch is not fixed in place, but is adjusted every few days while the defect is healing. At the Hospital Carlos Andrade Marin in Quito, the neonatal team sees 4 to 6 patients per year with Gastroschisis. The use of an umbilical cord patch enables them to close a large Gastroschisis defect in one step, instead of a series of stages. They find that surgery with an umbilical cord patch results in reduced healing time, decreased reliance on intravenous nutrition, faster discharge from the hospital, and better cosmetic outcomes7,8.
Spina Bifida is a birth defect where the spinal column does not close completely, leaving the spinal cord and nerves exposed or protruding9,10. This occurs once in about 2,000 births but requires surgical correction immediately after birth. We have previously published the story of Emma, a girl in Ukraine who was infused with her own cord blood as a compliment to her spina bifida surgery11. Despite surgery, children with spina bifida often have paralysis or limited use of their lower limbs. Research has shown that exposure of the spinal cord leads to progressive neurologic damage over the course of pregnancy. In order to intervene sooner and preserve mobility, the multi-center Management of Myelomeningocele Study (MOMS) NCT00060606 showed that in utero surgery to close the spinal cord leads to better outcomes12. Recently, a team at UC Davis in California registered a pioneering 2020 clinical trial NCT04652908 which combines in utero surgery for spina bifida with a patch consisting of a commercially available matrix that has been seeded with placental mesenchymal stromal cells (MSC).
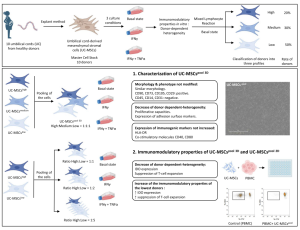
Research is ongoing to expand the use of birth tissues as a surgical patch. The team in Ecuador is studying the properties of the umbilical cord patch in order to make it more readily available and standardized for use in pediatric surgery8. Their current procedure is dependent on access to a fresh umbilical cord, and storage of this living tissue would be costly. They are studying the use of a decellularized umbilical cord that is seeded with a secretome containing growth factors. If this yields satisfactory surgical outcomes, it would make the use of umbilical cord surgical patches more widely accessible as an off-the-shelf surgical tool.
References:
- Children’s Hospital of Philadelphia. Umbilical Hernia.
- Children’s Hospital of Philadelphia. Congenital Diaphragmatic Hernia.
- CDH UK. What is CDH?
- Children’s Hospital of Philadelphia. Gastroschisis.
- Children’s Hospital of Philadelphia. Gastroschisis: Emma’s Story.
- Heaton FC, Thomas CG, Owen J. The use of umbilical cord for reconstruction of abdominal wall defects. Plastic and Reconstructive Surgery. 1971; 47(5):508.
- Zurita A, and Ocaña E. Cierre de la pared abdominal con parche de gelatina de Wharton en neonatos con gastrosquisis / Abdominal wall closure with Wharton’s gelatin patch in neonates with gastroschisis. VozAndes 2017; 28(1):15-19.
- Velarde F, Castañeda V, Morales E, Ortega M, Ocaña E, Álvarez-Barreto J, Grunauer M, Eguiguren L, Caicedo A. Use of Human Umbilical Cord and Its Byproducts in Tissue Regeneration. Front. Bioeng. Biotechnol. 2020; 8:117.
- Children’s Hospital of Philadelphia. Spina Bifida Causes, Symptoms and Treatment.
- UC Davis Health. First stem cell clinical trial for spina bifida treatment announced. Newsroom Published 2021-03-01
- Parent’s Guide to Cord Blood Foundation. Emma’s Story: Spina Bifida Surgery With Cord Blood. Newsletter Feb. 2020
- Farmer DL, Thom EA, Brock JW, Burrows PK, Johnson MP, Howell LJ, Farrell JA, Gupta N, Adzick NS. The Management of Myelomeningocele Study: full cohort 30-month pediatric outcomes. Amer. J. Obstetrics and Gynecology 2018; 218(2):256.e1-e13.
Source: Parent’s Guide to Cord Blood