News Medical & Life Sciences, Nov 22 , 2023
Reviewed by Lily Ramsey, LLM
In a recent article published in Molecules, researchers discuss using oncolytic viruses (OVs) in combination with nanomaterials as a novel approach to cancer treatment. Their combined use has the potential to overcome the limitations of each used individually, such as the side effects of OVs and the inadequate tumoricidal capacity of nanomedicines.
Additionally, they inquired about the working mechanisms and application of OVs in combination with nanomaterials and summarized scientific advancements to predict future trends in this critical research area.
Background
Despite substantial advancements in the diagnosis and treatment of cancer, enhancing their effectiveness while reducing side effects remains a daunting task.
For instance, gene-editing therapies utilizing viral vectors, such as adenoviruses and lentiviruses, successfully deliver therapeutic genes into target cancer cells; however, their effectiveness in certain tumors remains limited. Additionally, they carry risks, such as off-target mutations, which might provoke unexpected immune responses and ethical issues.
Oncolytic viruses and their therapeutic uses
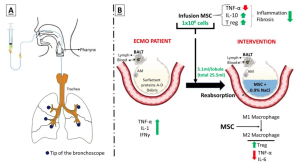
Tumor microenvironment (TME) effectively evades the immune system surveillance, thereby facilitating cancer growth and metastasis. One of the mechanisms involves the secretion of immunosuppressive agents, such as tumor growth factor-beta (TGF-β) and interleukin-10 (IL-10) by tumor cells, which directly inhibits immune cell activity.
Tumor cells can also recruit other immunosuppressive cells, such as myeloid-derived suppressor cells (MDSCs) and regulatory T-cells (Tregs), that suppress immune cells attacking the tumor.
OVs break through this immunosuppressive environment via two routes. First, they selectively infect and lyse tumor cells (direct lysis), which induces tumor cell apoptosis. Second, OVs can perform gene therapy. As an example, OVs carrying the granulocyte-macrophage colony-stimulating factor (GM-CSF) gene infect many tumor cells simultaneously, which then express this gene and recruit dendritic cells (DCs) and macrophages, which finally destroys tumor cells marked by antibodies post-infiltration.
When OVs are used with radiochemotherapy in tandem, both mutually enhance each other’s therapeutic effects. Radiochemotherapy reduces the immune suppression effects of tumor cells; thus, more OVs infect tumor cells.
This infiltration induces apoptosis in tumor cells, facilitating the deeper penetration of radio chemotherapeutic agents into the tumor mass, thus increasing their effectiveness. Additionally, OVs enhance anti-tumor immune responses, and with radiochemotherapy, they help overcome tumor resistance to treatment.
A remarkable example of the synergistic application of OVs and radiochemotherapy is the combined use of oncolytic Herpes Simplex Virus (HSV) and Temozolomide (TMZ), a radiochemotherapeutic agent, in a study by Fan et al.
They showed that this therapeutic approach diminished the viability of breast cancer cells, arrested the cell cycle, induced tumor cell apoptosis, and accentuated in vitro DNA damage response.
Similarly, when combined with immune checkpoint therapy, e.g., anti-Programmed Cell Death 1 (PD1)/Programmed Cell Death Ligand 1 (PD-L1) therapy, OVs convert ‘cold’ tumors to ‘hot’, which are more sensitive to immune checkpoint inhibitor therapy.
The innovation of Adoptive Cell Therapy (ACT) lies in providing cancer patients with enormous tumor-specific immune cells to help eliminate residual cancer cells. Preclinical studies have shown that OVs with ACT hold immense potential in various types of cancers.
For instance, Huang evaluated the in vitro and in vivo efficacy of OAd-IL7 and B7H3-CAR-T separately and in combination with glioblastoma. In mice, this treatment prolonged survival and reduced tumor burden.
Animal models have also shown the efficacy and sustainability of using bio nanocarrier viruses as a tumor treatment modality. For instance, the Human Papillomavirus (HPV) vaccine is an immune virus widely used to prevent cervical cancer. Similarly, virus-like particles (VLPs) are an attractive and safer alternative analogs of immune viruses. A study by Nooraei et al. showed that VLPs could also serve as nanocarriers for drugs.
Combination therapy with OVs and nanomaterials
Nanoparticle-based pre-treatment methods significantly enhance the efficacy of OV therapy. Surface-targeting ligand modification techniques improve the selectivity and infectivity of OVs.
Some examples include PEG modification (PEGylation), which reduces the likelihood of virus recognition by the host immune system.
Similarly, encapsulating Oncolytic Adenovirus (OAds) expressing TNF-related apoptosis-inducing ligand (TRAIL) within gelatin hydrogels prolongs OV’s anti-tumor activity.
Furthermore, combining ursolic acid nanoparticles (UA-NP) enhances the apoptotic cytotoxicity of oncolytic measles virus (MV) against breast cancer cells. An example of magnetic nanoparticles, another burgeoning frontier in cancer therapy, is PEG-coated magnetic iron oxide nanoparticles (MIONs) that encapsulate OAds.
These strategies are in continuous optimization; however, even little progress in this field indicates that the spectrum of OV application is broadening in cancer therapy.
Bio-nanocarriers are delivery systems that encapsulate drugs, genes, and immunotherapies into nano-scale carriers. Some examples are liposomes [CCL2 and polyethylene glycol (PEG)] and polymeric nanoparticles that encapsulate OVs, which enhance their stability within the target (patient) and promote their diffusion and release.
Many tumors have low immunogenicity against which lab-prepared CCL2-loaded liposomes have shown promising efficacy in mice.
They encapsulate the OAds, a novel immunotherapy strategy that enhances the infiltration and activation of monocytes in tumor tissues, anti-tumor immune response, and inhibits tumor growth.
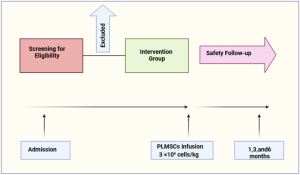
Likewise, mesenchymal stem cells (MSCs) are promising delivery vehicles that transport OVs directly to tumor sites. Additionally, their surface adhesion proteins can bind with nanoparticles, effectively cloaking them, an interaction that optimizes the release of OVs.
Furthermore, MSCs-derived extracellular vesicles (MSC-EVs) can help treat heart, liver, and neurological diseases. They also represent a safer, more stable alternative to MSCs for delivering anticancer drugs.
Some inorganic carriers, such as calcium-phosphate biomineralized OVs, enhance their stability and therapeutic activity, and adding magnetic iron oxide (FeO) nanoparticles to these helps target human osteosarcoma cells.
Magnetic bacteria-derived nanomagnets are another innovative approach that facilitates OVs entry to tumor tissues under the influence of an external magnetic field, thereby enhancing its therapeutic effects.
Conclusions
To conclude, viral therapy with nanomaterials achieves a synergistic effect and has the exceptional potential to revolutionize currently used cancer therapies.
Future research should focus on enhancing precision in tumor targeting, which requires advancements in OVs and nanomaterial design development and help realize the dream of precision cancer therapy in the future.
Increasing nanomaterial’s drug-carrying capacity could help improve therapeutic outcomes of cancer therapies without increasing dosages. However, addressing immune responses to these treatments is vital.
Journal reference:
- Li, H., Zhu, Y., Wang, X., Feng, Y., Qian, Y., Ma, Q., Li, X., Chen, Y., & Chen, K. (2023). Joining Forces: The Combined Application of Therapeutic Viruses and Nanomaterials in Cancer Therapy. Molecules, 28(22), 7679. doi: https://doi.org/10.3390/molecules28227679. https://www.mdpi.com/1420-3049/28/22/7679
Source: News Medical & Life Sciences