Plastic & Reconstructive Surgery – Global Open, 17/10/2025
Introduction
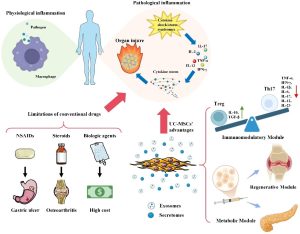
Chronic wounds, particularly those associated with diabetes, venous insufficiency, and smoking, present a persistent healthcare challenge characterized by impaired vascularity, prolonged inflammation, and delayed healing. Despite advances in wound care, conventional treatment modalities such as debridement, compression therapy, and topical agents frequently fail to achieve complete wound closure, highlighting the need for more effective interventions.
Exosomes are nanosized extracellular vesicles derived from various cell types that contain bioactive molecules crucial for cellular communication, inflammation modulation, and angiogenesis. Moreover, they support tissue regeneration through enhanced collagen deposition and extracellular matrix remodeling; therefore, exosome have the therapeutic potential in addressing the multifactorial deficits inherent in chronic wounds.
Method
- Selection criteria
- Presence of chronic wounds that had failed to respond to conventional treatments.
- Patients aged between 40 and 60 years with difficult-to-heal ulcers of varied etiologies (venous, arterial, hypertensive, diabetic, and mixed).
- All patients had wounds that persisted for at least 6 months despite standard therapy for their respective conditions.
- Pretreatment care and compliance
- Before initiating exosome therapy, all patients underwent comprehensive wound assessment and optimization of underlying conditions.
- The exosomes were isolated through a sequential ultracentrifugation process and suspended in a phosphate-buffered saline solution.
- Treatment protocol
- The treatment protocol involved monthly consultations for the application of exosomes (0.5–1 mL) directly onto the wound bed after thorough cleansing and debridement, if necessary. The volume of exosomes applied was adjusted according to wound size, with approximately 0.1 mL/cm2 of wound surface.
- After application, a 5- to 10-minute absorption period was observed before the wound was covered with a nonadherent, sterile dressing. Patients were instructed not to disturb the dressing for at least 24 hours after application.
- Wound assessment and follow up protocol
- Wounds were assessed at baseline and at each follow-up visit (every 2–4 week) using digital photography with a measurement scale to document changes in wound dimensions.
- Follow-up visits continued until complete wound closure was achieved or until the patient had received at least 6 months of treatment. At each visit, appropriate wound care was provided, and any adverse events or complications were recorded.
- Doppler studies
Arterial and venous Doppler ultrasonography was performed at baseline and at 3-month intervals during treatment to assess changes in vascular dynamics.
Results
Case 1: A 58-year-old woman with a long-standing history of diabetes and chronic venous insufficiency presented with a chronic ulcer that had persisted for more than 6 months. Previous conservative treatments, including compression therapy and topical wound care, resulted in only partial improvement.
After treatment:
- There was a reduction in wound size, accompanied by the development of healthy granulation tissue.
- Doppler ultrasound showed enhanced vascular dynamics in the treated area.
- The arterial resistive index decreased from 0.89 to 0.72, indicating improved distal flow, whereas venous reflux time decreased from 2.8 to 1.2 seconds, suggesting improved venous valve function.
Case 2: A 62-year-old woman presented with recurrent ulcers that had persisted for more than 2 years despite ongoing treatment with debridement and compression therapy.
After treatment:
- The wounds exhibited complete granulation and reepithelialization, with no evidence of inflammation or necrosis.
- Doppler ultrasound performed at baseline and 3 months after treatment initiation confirmed enhanced vascular permeability and improved local perfusion, correlating with the clinical improvement seen during the follow-up.
- Peak systolic velocity increased from 28 to 42 cm/s, whereas the resistive index decreased from 0.92 to 0.78.
Case 3: A 42-year-old man with a 6-year history of chronic venous insufficiency and recurrent ulcers was referred after the failure of traditional nonsurgical treatments to achieve significant improvement.
After treatment:
- The ulcers demonstrated substantial closure, with evident healthy tissue regeneration and a marked reduction in inflammatory signs.
- The wounds had nearly resolved, with complete granulation and restored skin integrity.
- Doppler imaging throughout the treatment period revealed progressive improvements in vascular dynamics, including reduced resistance and enhanced blood flow to the affected area.
- Patient’s resistive index was improved from 0.95 at baseline to 0.81 at 3 months and 0.75 at 6 months.
- Venous reflux time decreased from 3.2 to 1.6 seconds.
Case 4: A 44-year-old woman presented with a chronic ulcer extending from the dorsum of the left foot to the second toe, a condition that developed after cellulitis or erysipelas. The severity of the wound and its failure to respond to conventional treatment prompted a recommendation for amputation.
After treatment:
- The ulcer achieved complete closure, with restored skin integrity and resolution of inflammation.
- Doppler ultrasound findings demonstrated significant vascular regeneration, with restored perfusion to previously ischemic areas.
- Peak systolic velocity increased from 15 to 38 cm/s, and end-diastolic velocity improved from 2 to 12 cm/s.
- The resistive index decreased from 0.97 to 0.82.
Discussion
By promoting angiogenesis, modulating the inflammatory response, and supporting tissue regeneration, exosomes have demonstrated the potential to accelerate healing in chronic wounds, even in high-risk patients with underlying comorbidities. Combining exosome therapy with maintaining good nutrition and healthy lifestyle may significantly improve clinical outcomes and the overall healing process.
Challenges of exosome therapy:
- Entails a more rigorous approval process before they can be marketed for clinical use.
- Exosomes must be stored at low temperatures (−20°C to −80°C) and used promptly after thawing to prevent degradation.
- Clinical studies supporting such dramatic improvements in Doppler-based vascular dynamics are currently limited.
- Patient characteristics and wound type may significantly influence therapeutic outcomes, emphasizing the need for personalized treatment protocols.
Study limitations:
- Small sample size
- Lack of a control group
- Absence of objective imaging
- Findings are preliminary and primarily observational, making it difficult to draw definitive conclusions regarding efficacy or mechanism.
- Standardized outcome measures and long-term follow-up were not used.
Conclusion
This case series demonstrates promising results for exosome therapy in chronic wound management, offering a targeted approach to address the underlying factors that impede healing in high-risk patients. The observed improvements in wound healing and vascular parameters suggest potential clinical benefit, although larger controlled studies are needed to establish definitive efficacy. With further clinical validation and regulatory approval, exosome therapy could provide an alternative option for patients with chronic wounds that have not responded to traditional treatments.
References
Basamage, L., Ahn, H. J., Choi, H.-S., Antonio, C. R., Alarcão, A. L., Silva, S. N., Hohl, Z. T., Wan, J., & Yi, K.-H. (2025). Exosome therapy for chronic wound healing. Plastic & Reconstructive Surgery – Global Open, 13(10), e7200.
Source: Plastic & Reconstructive Surgery – Global Open
Link: https://journals.lww.com/prsgo/fulltext/2025/10000/exosome_therapy_for_chronic_wound_healing.31.aspx?context=latestarticles