DVCSTEM, May 12, 2023
Louis A. Cona, MD
Mesenchymal stem cells (MSCs) are adult stem cells with the ability to differentiate into various types of mesoderm-derived cells, showing promising results in preclinical studies for various medical conditions. Research continues to explore their potential in regenerative medicine.
What are Mesenchymal Stem Cells (MSCs)?
Mesenchymal stem cells (MSCs) are adult stem cells isolated from different sources that can differentiate into other types of cells. Sources of MSCs include bone marrow, fat (adipose tissue), and umbilical cord tissue.
Mesenchymal stem cells (MSCs) can self-renew and also exhibit multilineage differentiation. They can supplement a person’s stem cell count through transplants, as they can avoid a negative response from a person’s immune system[1].
Mesenchymal stem cells (MSCs) have become widely studied for their unique cell biology, broad-ranging clinical potential, and as a central building block in the rapidly growing field of tissue engineering[4]. Clinical studies investigating the efficacy of mesenchymal stem cells in treating diseases are in preliminary development, particularly for understanding autoimmune diseases, graft versus host disease, and cancer. The International Society for Cellular Therapy (ISCT) has proposed standards to define Mesenchymal Stem Cells (MSCs).
What does mesenchymal mean?
The term “mesenchymal” refers to the embryonic origin of the cells, specifically cells that arise from the mesoderm germ layer. The mesoderm germ layer is one of the three primary germ layers that form during the early stages of embryonic development. The mesoderm gives rise to various types of connective tissues, such as muscle, bone, cartilage, and fat, as well as the cells that form blood vessels, blood cells, and the urogenital system.
What characteristics define human mesenchymal stem cells?
The International Society for Cellular Therapy’s Mesenchymal and Tissue Stem Cell Committee suggests minimal standards for identifying human Mesenchymal Stem Cells (MSCs).
First: A mesenchymal stem cell (MSC) must be plastic-adherent when maintained in standard culture conditions.
Second: A mesenchymal stem cell (MSC) must express CD105, CD73, and CD90 and lack expression of CD45, CD34, CD14 or CD11b, CD79α or CD19, and HLA-DR surface molecules.
Third: A mesenchymal stem cell (MSC) must differentiate into osteoblasts, adipocytes, and chondroblasts in vitro.
Although the criteria for identifying mesenchymal stem cells (MSCs) may need to be adjusted as new knowledge emerges, it is believed that the minimum standards proposed by the ISCT will lead to the more consistent characterization of mesenchymal stem cells (MSCs) and facilitate collaboration among researchers.
Currently, mesenchymal stem cell (MSC) research is hindered by various methods and approaches for cell isolation, expansion, and characterization, making it difficult to compare and contrast study outcomes. The ISCT guidelines aim to standardize mesenchymal stem cell research.
Differentiation potential of mesenchymal stem cells (MSCs)
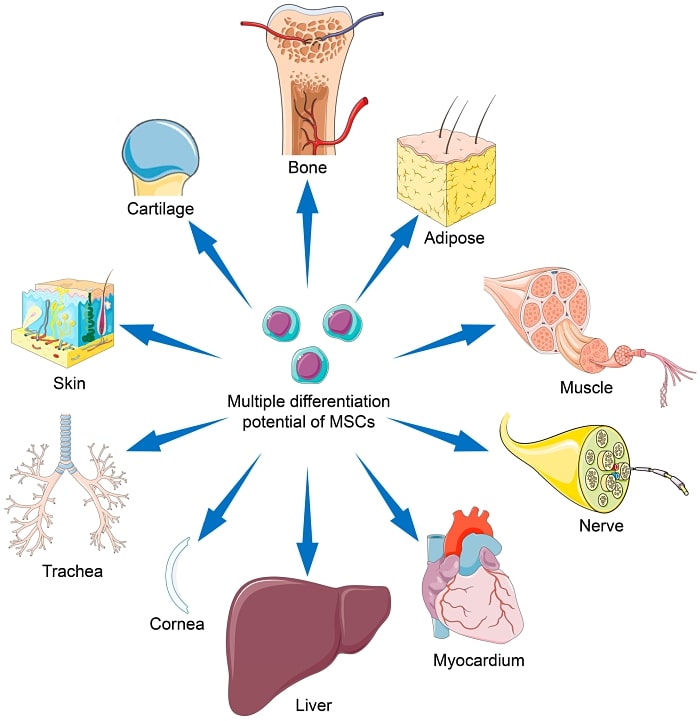
Mesenchymal stem cells (MSCs) are a type of adult stem cell that can differentiate into a variety of cell types, including osteoblasts (bone cells), chondrocytes (cartilage cells), and adipocytes (fat cells). Human mesenchymal stem cells can also differentiate into other cell types, such as myocytes (muscle cells), neurocytes (nerve cells), and stromal cells.
According to a peer-reviewed study published in the journal Stem Cell Reviews and Reports (3), mesenchymal stem cells (MSCs) have been shown to differentiate into various cell types, including:
Osteoblasts (bone cells)
Chondrocytes (cartilage cells)
Adipocytes (fat cells)
Myocytes (muscle cells)
Neurocytes (nerve cells)
Hepatocytes (liver cells)
Pancreatic cells (pancreas cells)
Cardiomyocytes (heart muscle cells)
Endothelial cells (blood vessel cells)
Epithelial cells (cells that line surfaces)
In another peer-reviewed study published in the International Journal of Molecular Sciences, mesenchymal cells can differentiate into mesodermal lineage cells, including osteoblasts, adipocytes, and chondrocytes as cells of ectodermal and endodermal origin, such as neurocytes, and in hepatocytes, respectively. (4)
It’s important to note that the differentiation potential of mesenchymal stem cells (MSCs) may vary depending on the source of the stem cells, the expansion conditions, and the microenvironment in which they are cultured.
What is differentiation potential?
Differentiation is when a less specialized cell becomes a more specialized cell type. In mesenchymal stem cells, differentiation refers to the process by which stem cells become specific cell types, such as muscle cells, nerve cells, or bone cells.
A complex interplay of genetic and epigenetic factors controls the differentiation process. Genetic factors include the expression of specific transcription factors and signaling molecules, while epigenetic factors include changes in DNA methylation, histone modification, and non-coding RNA expression.
The process of differentiation can be divided into several stages. The first stage is the activation of specific genes, which leads to the expression of transcription factors that control the cell’s fate. The second stage is the initiation of cell proliferation and the formation of specific cell types. The final stage is the maturation of the cells, which leads to the formation of functional cells.
Various factors can influence differentiation potential
Various factors, such as the microenvironment, the availability of growth factors, and the presence of other cells, can influence the differentiation process. For example, specific signaling molecules, such as bone morphogenetic proteins (BMPs) or Wingless-related integration sites (Wnts), can promote the differentiation of stem cells into bone cells or nerve cells, respectively.
In the case of MSCs or multipotent mesenchymal stromal cells, the differentiation process can be induced by differentiating agents such as specific growth factors, hormones, or chemical compounds in a defined culture medium. The differentiation potential of mesenchymal stem cells (MSCs) may vary depending on the source of the cells, the expansion conditions, and the microenvironment in which they are cultured.
What is the function of mesenchymal stem cells (MSCs)?
Differentiation potential
Mesenchymal stem cells (MSCs) have a wide range of functions, which include the ability to differentiate into various cell types, such as osteoblasts (bone cells), chondrocytes (cartilage cells), and adipocytes (fat cells). Additionally, mesenchymal stem cells (MSCs) can inhibit the immune response and promote tissue repair.
Immunomodulatory properties
Mesenchymal stem cells (MSCs) are known for their immunomodulatory properties, which means they can modulate the activity of the immune system, reduce inflammation and suppress immune responses. This property makes them a promising candidate for cell-based therapies in various conditions, such as autoimmune diseases, graft-versus-host disease, and transplant rejection.
Promote tissue repair and regeneration
Mesenchymal stem cells (MSCs) also can promote tissue repair by releasing growth factors and cytokines, which help recruit other cells to the injury site. These growth factors and cytokines can also promote the formation of new blood vessels essential for tissue repair.
Mesenchymal stem cells (MSCs) are also being evaluated in preclinical and clinical studies to treat diseases such as osteoarthritis, osteogenesis imperfecta, Crohn’s Disease, Multiple Sclerosis, Parkinson’s, and many others.
It’s important to note that while Mesenchymal stem cells (MSCs) have shown promising results in preclinical studies, more research is needed to understand their potential fully and to develop safe and effective therapies.
Where are mesenchymal stem cells (MSCs) found?
There are several sources of mesenchymal stem cells (MSCs), including:
- Bone Marrow is the most commonly used Mesenchymal stem cell (MSCs) source. Bone marrow is the spongy tissue inside the bones that contains immature cells, including MSCs. These cells can be collected through a procedure called bone marrow aspiration, which is a relatively simple and safe procedure.
- Adipose Tissue (Fat Tissue): Mesenchymal stem cells (MSCs) can also be isolated from adipose tissue, which is the tissue that stores fat in the body. Adipose tissue can be obtained through liposuction, a procedure in which fat is removed from the body using a hollow stainless steel tube.
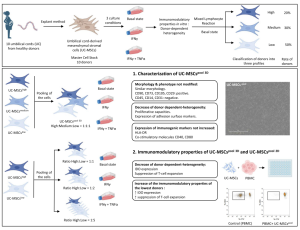
- Umbilical Cord Tissue: Mesenchymal stem cells (MSCs) can also be obtained from umbilical cord tissue, which is the tissue that connects the fetus to the placenta. The cells can be collected at the time of birth and can be stored for future use.
- Peripheral Blood: Mesenchymal stem cells (MSCs) can be found in small numbers in the peripheral blood of healthy adults. These cells can be collected through a procedure called apheresis, which is similar to donating blood.
- Placental Tissue: Mesenchymal stem cells (MSCs) can also be obtained from placental tissue. The cells can be collected at the time of birth and can be stored for future use.
- Synovial Fluid: Mesenchymal stem cells (MSCs) can be found in small numbers in the synovial fluid of joints. Synovial fluid can be obtained through a procedure called arthrocentesis, which is a relatively simple and safe procedure.
- Dental Pulp: Mesenchymal stem cells (MSCs) can be found in small numbers in the dental pulp of teeth. Dental pulp can be obtained through a procedure called apicoectomy, which is a surgical procedure to remove the tip of a tooth’s root.
The cells derived from cord tissue, specifically Wharton’s Jelly, are the youngest and most primitive MSCs available. With most umbilical cords discarded after childbirth, this source is non-harmful and readily available—view the source article.
It is critical to note that the isolation and expansion of MSCs from different sources may vary and have other properties. Also, isolating MSCs from some locations, such as Peripheral blood and synovial fluid, maybe more challenging and less efficient than bone marrow, adipose tissue, or umbilical cord tissue-derived mesenchymal stem cells (MSCs).
What are the disadvantages of mesenchymal stem cells (MSCs)?
While mesenchymal stem cells (MSCs) and multipotent stem cells have shown promising results in preclinical studies, there are also several limitations and challenges associated with their use in research:
- Heterogeneity: MSCs from different sources, such as bone marrow and adipose tissue, may have other properties and may not be completely interchangeable. This can make it difficult to compare results from various studies.
- Variability in isolation and expansion: The isolation and expansion of MSCs from different sources may vary and may have other properties, making it difficult to replicate results from one study to another.
- Limited differentiation potential: While MSCs can differentiate into various cell types, their differentiation potential may vary depending on the source of the cells, the expansion conditions, and the microenvironment in which they are cultured.
- Quality control: There is a need for standardized methods for the isolation, expansion, and characterization of MSCs, which can help to ensure the quality and consistency of the cells used in research.
- Safety and efficacy: While MSCs have shown promising results in preclinical studies, more research is needed to understand their potential and develop safe and effective therapies fully.
Mesenchymal stem cells (MSCs) vs Hematopoietic stem cells (HSCs)
Mesenchymal stem cells (MSCs) and hematopoietic stem cells (HSCs) are both adult stem cells but have distinct differences.
- Differentiation potential: Mesenchymal stem cells (MSCs) can differentiate into a variety of cell types, such as osteoblasts (bone cells), chondrocytes (cartilage cells), and adipocytes (fat cells), as well as other cell types, such as myocytes (muscle cells), neurocytes (nerve cells), and stromal cells. In contrast, HSCs primarily differentiate into blood cells and cells of the immune system, such as red blood cells, white blood cells, and platelets.
- Source: Mesenchymal stem cells (MSCs) can be isolated from various sources such as bone marrow, adipose tissue, umbilical cord, peripheral blood, placental tissue, synovial fluid, and dental pulp. On the other hand, HSCs are primarily obtained from bone marrow but can also be found in small numbers in the peripheral blood.
- Immune properties: Mesenchymal stem cells (MSCs) have immunomodulatory properties, which means they can modulate the activity of the immune system, reduce inflammation and suppress immune responses. HSCs, on the other hand, are responsible for producing and maintaining immune system cells, so they don’t have the same kind of immune modulatory properties.
- Therapeutic applications: Mesenchymal stem cells (MSCs) have been studied for many therapeutic applications, including tissue repair, regenerative medicine, and cell-based therapies for various diseases. HSCs, on the other hand, have been primarily used for treating blood disorders such as leukemia, lymphoma, and sickle cell anemia, as well as for bone marrow transplantation.
It’s important to note that Mesenchymal stem cells (MSCs) and HSCs are complex cell types, and there is still much to be learned about their properties and potential therapeutic applications.
What medical conditions can mesenchymal stem cells be used for?
Mesenchymal stem cells (MSCs) have been studied for a wide range of therapeutic applications, including tissue repair, regenerative medicine, and cell-based therapies for various medical conditions. Some of the medical conditions that MSCs have been studied for include:
- Osteoarthritis: the promotion of cartilage repair and reduced inflammation in osteoarthritis, a degenerative joint disease that affects the cartilage and bone in the joints.
- Rheumatoid arthritis: anti-inflammatory and immunomodulatory properties that may be useful in treating rheumatoid arthritis. This autoimmune disorder causes inflammation and damage to the joints.
- Graft-versus-host disease: immunosuppressive properties may make MSCs useful in treating graft-versus-host disease. This complication can occur after a bone marrow transplant.
- Myocardial infarction: MSCs have been studied for their potential to promote heart tissue repair following a heart attack.
- Spinal cord injury: MSCs have been investigated for their potential to promote the repair of damaged nerve tissue and spinal cord injury
- Autoimmune diseases: MSCs have been demonstrated to have anti-inflammatory and immunomodulatory properties, which may make them helpful in treating autoimmune diseases, such as multiple sclerosis and lupus.
- Type 1 diabetes: MSCs have been examined for their potential to help preserve insulin-producing cells in type 1 diabetes patients
- Lung diseases: MSCs have been reviewed for their potential to help repair lung tissue in conditions such as chronic obstructive pulmonary disease (COPD) and acute respiratory distress syndrome (ARDS).
- Multiple Sclerosis (MS): MSCs have been shown to have anti-inflammatory and immunomodulatory properties, which may make them helpful in treating MS. This autoimmune disorder affects the central nervous system.
- Lyme Disease: MSCs have been analyzed for their potential to help repair tissue damage and reduce inflammation caused by Lyme disease, a bacterial infection transmitted by ticks.
- Parkinson’s Disease: MSCs have been examined for their potential to help protect and repair nerve cells in the brain that are damaged in Parkinson’s disease, a degenerative disorder that affects movement.
- ALS (Amyotrophic lateral sclerosis): MSCs have been investigated for their potential to help protect and repair nerve cells in the spinal cord damaged in ALS, a progressive neurodegenerative disease that affects nerve cells in the brain and spinal cord.
It’s important to note that while MSCs have shown promising results in preclinical studies, more research is needed to understand their potential fully and to develop safe and effective therapies. Additionally, the use of MSCs as a therapy is still considered. The medical community has known of the existence of MSCs since the late 19th century. However, it has only been with recent advancements that physicians have been able to activate and supplement these cells to treat various conditions.
References:
(1) Ullah, I., Subbarao, R. B., & Rho, G. J. (2015, April 28). Human mesenchymal stem cells – current trends and future prospective. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4413017/.
(2) Ding DC, Shyu WC, Lin SZ. Mesenchymal stem cells. Cell Transplant. 2011;20(1):5-14. doi: 10.3727/096368910X. PMID: 21396235.
(3) Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR. Multilineage potential of adult human mesenchymal stem cells. Science. 1999 Apr 2;284(5411):143-7. doi: 10.1126/science.284.5411.143. PMID: 10102814.
(4) Williams AR, Hare JM. Mesenchymal stem cells: biology, pathophysiology, translational findings, and therapeutic implications for cardiac disease. Circ Res. 2011 Sep 30;109(8):923-40. doi: 10.1161/CIRCRESAHA.111.243147. PMID: 21960725; PMCID: PMC3604746.
(5) Mesenchymal Stem Cells: Biology, Pathways, Translations, and Therapeutic Implications” R. Mishra and S.A. Pittenger, International Journal of Molecular Sciences, 2019.
(6) Comparison of bone marrow- and adipose tissue-derived mesenchymal stem cells: a systematic review” by L. Huang, Y. Liu, P. Cui, and L. Li, Stem Cell Reviews and Reports, 2010.
(7) Standardization of mesenchymal stem cell isolation, expansion and characterization” by C.D. Corcione, R. De Bari, and M.L. Lazzari, Journal of Cellular and Molecular Medicine, 2009.
Source: DVCSTEM
Link: https://www.dvcstem.com/post/what-are-mesenchymal-stem-cells