University of California San Francisco, August 31, 2020
Researchers are studying whether cells drawn from deep inside our bones may hold hope for the sickest of COVID-19 patients who have severe lung injury called acute respiratory distress syndrome, or ARDS.
The clinical trial, led by Michael Matthay, MD, of UC San Francisco, is testing the effects of infusions of stem cells drawn from bone marrow in the hopes of finding a therapy for the deadly syndrome.
For a patient suffering from ARDS, “tiny air spaces in the lungs fill up with fluid and prevent normal oxygen uptake in the lungs,” said Michael Matthay, MD, professor of medicine at the UCSF School of Medicine. “That’s why the patient has respiratory failure. Usually these patients have to be intubated and treated with a mechanical ventilator.”
There is not currently any drug to treat ARDS, which has a mortality rate of 27 percent for mild cases and 45 percent for the most severe cases. An early study on COVID-19 patients with ARDS found that only about 25 percent survive, though that percentage may be as high as 40 percent, according to Matthay.
Patients in a randomized double blind clinical trial are being given mesenchymal stem cells (MSCs) or placebo to test the effectiveness of the therapy. The trial – ongoing at UCSF, Zuckerberg San Francisco General Hospital, and soon to expand to UC Davis and four other sites in September – hopes to repair the severe and often fatal lung damage in people suffering from ARDS.
“It’s a very interesting possible therapy,” said Matthay. “We’re really in the early phases of understanding these cell-based therapies.”
Cells That Can Modulate Inflammation
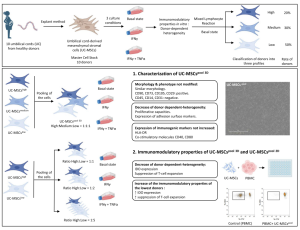
MSCs are stromal cells found in bone marrow, play a key role in how our bodies make and repair skeletal tissues – things like bone and cartilage and support the cells in the bone marrow that produce red and white blood cells. Once researchers discovered that MSCs could modulate inflammation when transplanted into other people, they began exploring them as potential therapies for a range of diseases and traumas.
For example, MSCs are often used to stop graft versus host disease, which is when transplant patients from rejecting new organs or bone marrow. More recent studies have focused on an array of potential disease targets because MSCs “have properties that may be useful to treat a variety of human illnesses,” said Matthay. Those include autoimmune diseases like Crohn’s disease and multiple sclerosis, and severe, acute conditions like sepsis and ARDS.
ARDS can be caused by trauma, bacterial infection, or a viral infection like COVID-19. In an earlier trial, Matthay and his team showed that MSCs are be safe to use, and that they have promising benefits in treating patients with ARDS. But they do not know how effective the MSC infusions are, and if results vary depending on what caused ARDS in the first place. Would they work better in a patient whose ARDS was caused by trauma? Or maybe they work better in concert with antibiotics used to treat ARDS that was set off by a bacterial infection.
“ARDS is a syndrome of acute respiratory failure that we understand reasonably well, but there’s a lot of heterogeneity in terms of the different mechanisms of injury to the lung and also outcomes,” he said.
Study Turned to COVID-19 Post Outbreak
In this Phase 2 double blind clinical trial – being funded by the Department of Defense, the National Institutes of Health, and the California Institute of Regenerative Medicine – researchers are enrolling 120 ARDS patients. Enrollees are adult ICU patients who are on ventilators with excess fluid in their lungs, and no sign of heart failure as a primary cause of the respiratory failure.
Half of the patients will receive MSCs and half a placebo. As of late August, 28 patients were enrolled in the study, which will run until researchers reach 120 enrollees. The MSCs used in the study have been donated by young, healthy adults via an NIH-supported cell laboratory at the University of Minnesota.
When Matthay launched a new study in early January, he didn’t expect it be a COVID trial. That’s because COVID – as far as was known then – wasn’t in the U.S. But that’s exactly what it inadvertently became since many patients who met the ARDS study criteria were suffering the condition because of COVID-19.
“We started the study in January 2020, and then COVID-19 hit, so we have been enrolling patients over the last eight months,” he said. “Most of the patients we’ve enrolled in the trial have ended up having severe viral pneumonia from COVID.”
Based on these outcomes and further studies on MSCs, Matthay sees them as a possible route for cell-based therapy. Much like cancer treatment isn’t one approach but instead different therapies tailored to the type of cancer cells, use of something like MSCs could be perhaps tailored exactly to whatever specific kind of syndrome of respiratory failure.