Umbilical cord blood may be a good alternative to bone marrow transplants for treating HIV in patients with HIV and cancer.
The Scientist, March 16th 2022
A woman in the New York City area appears to be the third person and the first woman ever to be cured of an HIV infection following a new stem cell transplant treatment involving umbilical cord blood. She has shown no detectable signs of the virus since stopping antiretroviral treatment in October 2020.
Her doctors presented the case on Tuesday (February 15) at the Conference on Retroviruses and Opportunistic Infections in Denver, but the findings have not yet been published.
“Everything is looking very promising,” Marshall Glesby, the chief of the division of infectious diseases at Weill Cornell Medicine and New York-Presbyterian, who treated the woman, tells The Wall Street Journal.
According to The New York Times, the woman was diagnosed with HIV in 2013. In March 2017, she was diagnosed with acute myeloid leukemia, which made her a candidate for a stem cell transplant, according to the Journal.
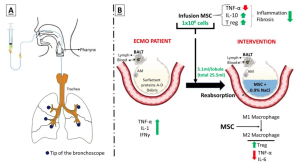
Later that year, she received a stem cell transplant in the form of two blood transfusions: one from an adult relative and the other of umbilical blood from an unrelated newborn. The newborn, who was a partially matched donor, had a mutation in a gene called CCR5, which hinders HIV’s ability to invade host cells, according to the Journal. The woman and her doctors discontinued her HIV treatment in 2020, three years after her transplant, and she has yet to show any detectable signs of the virus in the months since. She has also been in cancer remission for more than four years.
Roughly 38 million people live with HIV worldwide and about 73 percent of them are receiving treatment in the form of antiretroviral therapy, but only three have been cured.
Umbilical cord blood transplants usually don’t serve as a treatment for cancer since they can take up to six weeks to engraft and because there are typically few stem cells in the cord. That’s why her doctors implanted the adult stem cells, which gave her body temporary immune defenses while the umbilical cord blood cells replicated and eventually replaced the adult stem cells, reports the Journal.
Since umbilical blood is more readily available than bone marrow, researchers say the treatment could likely help other patients as well, reports the Times. The umbilical cord cells don’t need to be genetically matched as closely to the recipient as bone marrow cells do and could potentially improve treatment options for people with both cancer and HIV. However, these transplants are unlikely to benefit HIV patients who don’t also have other diseases such as cancer, HIV researcher Sharon Lewin, who’s the director of the Peter Doherty Institute for Infection and Immunity in Melbourne, Australia, and was not involved in the work, tells the Journal.
“We estimate that there are approximately 50 patients per year in the US who could benefit from this procedure,” Koen van Besien, one of the doctors involved in the treatment, tells The Guardian.
The two other patients who beat HIV—also cancer patients—received bone marrow stem cell transplants that also carried a CCR5 mutation. But bone marrow transplants are rare because they can have severe side effects, reports the Times. Both previous patients whom scientists cured of HIV developed graft versus host disease, a debilitating condition where the donor’s cells attack the recipient’s body. One patient nearly died; the other lost almost 70 pounds and developed hearing loss.
By contrast, the recently-cured woman left the hospital 17 days later and did not develop graft versus host disease.
“It was previously thought that graft versus host disease might be an important reason for an H.I.V. cure in the prior cases,” Lewin tells the Times. The new results counter the idea that graft versus host disease is an inevitable aspect of HIV cures, Lewin says.
The scientists behind the treatment tell the Guardian that most donors included in registries are of Caucasian descent. In contrast, the woman is of mixed race. As a result, they say, allowing for umbilical cord transplantations that are only partial matches might open treatment options for patients with both HIV and cancer who come from more diverse backgrounds.
“The fact that she’s mixed race, and that she’s a woman, that is really important scientifically and really important in terms of the community impact,” Steven Deeks, an HIV researcher at the University of California, San Francisco, who was not involved in the work, tells the Times.
The scientists aren’t sure why the umbilical cord blood works so well, experts tell the Times. One possibility is that umbilical stem cells are more capable of adapting than bone marrow stem cells, says Koen Van Besien, director of the transplant service at Weill Cornell. “These are newborns, they are more adaptable,” he says.
Umbilical cord blood may also contain therapeutic elements other than the stem cells, according to the Times.
“Umbilical stem cells are attractive,” Deeks tells the Times. “There’s something magical about these cells and something magical perhaps about the cord blood in general that provides an extra benefit.”
Source: The Scientist